|
|
|
New 2026 benefit: contact lens allowance
AmeriHealth Caritas Ohio members will have access to a new Value-added Service: Up to $150 toward the purchase of contact lenses each calendar year.
To qualify, members must:
- Complete an eye exam
- Receive contact lens fitting
- Have a valid contact lens prescription
What Providers Need to Know:
Please ensure members receive the required eye exam and fitting, and that prescriptions are current and documented. This will help members take full advantage of their new benefit and keep their vision clear and healthy!
|
|
|---|
|
HEDIS records request
HEDIS® is a national set of quality measures that helps health plans and providers understand how well members are receiving important care and services. State and federal agencies use HEDIS results to monitor quality, support accreditation, and compare performance across health plans. The information collected each year also helps identify opportunities to improve care for the communities we jointly serve.
Each year from January through April, AmeriHealth Caritas Ohio conducts medical record reviews for a small group of members whose claims data show
|
|
|
missing information or possible care gaps. During this time, you may receive requests for medical records needed to complete this review.
To support this year’s process, AmeriHealth Caritas Ohio has partnered with PalmQuest, who will coordinate the medical record retrieval on our behalf.
We sincerely appreciate your partnership and your timely assistance in responding to these requests. Your support helps ensure accurate quality reporting and better outcomes for our members.
|
|
|---|
|
Engage, Empower, Treat: A Behavioral Health ECHO Learning Series
AmeriHealth Caritas Ohio, in collaboration with Project ECHO, is excited to launch an emerging case-based learning model for practitioners. Continuing Education for participants who participate in this series will be applied through Arizona State University, for physicians and nurses, and the Ohio Counselor, Social Worker, and Marriage and Family Therapist (CSWMFT) Board for social workers, licensed professional counselors, and marriage and family therapists. This opportunity doesn’t cost anything for participating AmeriHealth Caritas Ohio practitioners.
For registration instructions, email: projectecho@amerihealthcaritas.com.
|
Date
|
Topic
|
|
February 12
Noon to 1 p.m.
|
Empowering People with Developmental Disabilities
|
|
March 12
Noon to 1 p.m.
|
Reframing Addiction: A Chronic Disease Approach to Treatment and Recovery
|
|
April 9
Noon to 1 p.m.
|
Zero Suicide using the Trauma Informed Care Model
|
|
May 14
Noon to 1 p.m.
|
Managing Behavioral Health Conditions During the Perinatal Period
|
|
June 11
Noon to 1 p.m.
|
Attention Deficit Hyperactivity Disorder (ADHD) in Adults
|
|
July 9
Noon to 1 p.m.
|
Start the Conversation: Assessment and Intervention for Alcohol Use
|
|
|
|---|
|
Ohio Department of Medicaid (ODM) updates
To stay up to date on ODM news, subscribe to the ODM Press.
Orthodontic Evaluation Form 03630 update
- The Ohio Department of Medicaid revised Form 03630 in September 2025 for a January 1, 2026, effective date. The “Revised ODM Form 03630” replaces all previously existing versions of Form 03630 and their included criteria.
- The new Ortho process went into effect January 1 and will be REQUIRED on all cases submitted moving forward.
- The updated form can be accessed directly from the ODM website: ODM 03630 - Referral Evaluation Criteria for Comprehensive Orthodontic Treatment
Billing codes
ODM has provided guidance on billing codes for multiple births through Medicaid Advisory Letter (MAL) No. 685. This MAL can be found here.
With the new integrated Ohio Medicaid Enterprise System (OMES), delivery codes for multiple births should be reported on separate details on the claim with modifier 51 appended.
Modifiers
The Modifiers Recognized by Ohio Medicaid Fee-For-Service document has been updated. Have questions on what the correct modifier is to use for a service or supply procedure? ODM’s website has a list of approved modifiers.
Tips for contacting the Ohio Medicaid Integrated Helpdesk
The Integrated Helpdesk (IHD) is a great resource to use when you run into an issue. It provides 24-hour, seven days a week access to information regarding client eligibility, claim and payment status, and provider information. Call 1-800-686-1516 or email IHD@medicaid.ohio.gov.
Provider education and training resources
It is important that providers update all 1099 address information in the Provider Network Management (PNM) module regularly. Ensure all information is current, including extra address details like suite number, house/office number, etc. to reduce the chance of non-delivery by the postal service. Access the quick reference guides here.
|
|
|---|
|
Ohio Department of Medicaid email links
|
|
|---|
|
 Claims and billing Claims and billing |
|
|---|
|
Questions about reimbursement or payment policies?
Click the appropriate link below for more detailed information.
Clinical Policies
Electronic claims submission
Providers can choose the submission option that works for them. It can be any approved clearinghouse or direct to ODM. Preferred options are:
- Availity (subscription)
- Change Healthcare (no cost)
Claim attachments
Step 1: Go to Availity attachment portal, send the attachments first. Make sure the “Attachment Control #” is unique to that claim and make note of it. E.g., if they are sending three attachments then, Attachment A – 111111, Attachment B – 22222, …
Step 2: Go to Change Healthcare's portal, ConnectCenter. When keying in the claim, in the attachment section, add the “Attachment Control #” which they noted (111111, 222222, ...). And from the drop-down menu choose the right “Attachment type.”
Note: “Attachment Control #” must be unique for that claim. You can add Member name or anything, but it must be unique for that claim. In other words, you can use 111111, 222222, … for the second claim you are submitting.
NaviNet pro tips
Claims Investigations
- If a provider has multiple offices or TINs, users must be linked to each TIN for the corresponding office to view claims and remittance advice.
How to file a Dispute in NaviNet
Electronic funds transfer
AmeriHealth Caritas Ohio has contracted with Change Healthcare and ECHO® Health, Inc., to administer electronic funds transfer (EFT) payments. There are no fees for single payer agreements to receive a direct payment from AmeriHealth Caritas Ohio via EFT or to receive an electronic remittance advice (ERA). Click to learn how to enroll, the payment schedule, and more.
Claims Payment Systemic Error report
The Claims Payment Systemic Errors (CPSE) report is updated and posted monthly on our website. AmeriHealth Caritas Ohio encourages you to review this log frequently and before contacting our Provider Services team. If you have additional questions, please reach out to Provider Services at 1-833-644-6001 and, as always, you can reach out to your local account executive.
Dispute or appeal?
If a provider disagrees with the outcome of a claim, the first step should always be to submit a claim dispute.
Provider disputes
Provider claim disputes are any provider inquiries or requests for reconsiderations, ranging from general questions about a claim to a provider disagreeing with a claim denial. Provider Dispute Submission Form (PDF)
A dispute can be submitted using any of the following methods:
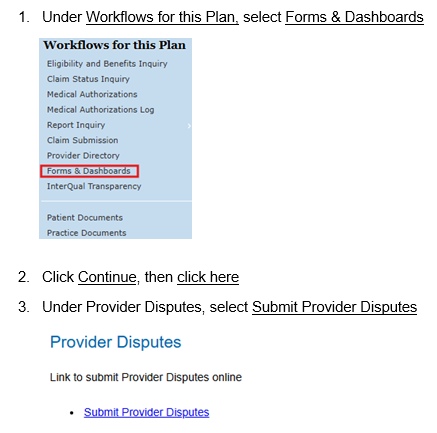
- NaviNet (recommended method): Providers can submit a dispute with attachments to AmeriHealth Caritas Ohio via NaviNet instead of faxing or mailing. Log in, go to Forms & Dashboards, scroll down to Provider Disputes, click the Submit Provider Disputes link. The turnaround time is 15 days for disputes.
- Mail the form with your supporting documentation to:
AmeriHealth Caritas Ohio
Attn: Provider Claim Inquiry
P.O. Box 7126
London, KY 40742
- Phone: 1-833-644-6001. Select the prompts for the correct department and then select the prompt for claim issues.
- Fax: 1-833-216-2272
Provider appeals
Providers may file an appeal on a denied pre-service within 30 days of the notice of Adverse Benefit Determination (ABD).
- Mail the form with your supporting documentation to:
AmeriHealth Caritas Ohio
Attn: Provider Claim Inquiry
P.O. Box 7400
London, KY 40742
- Fax: 1-833-564-1329
Best practices to ensure accurate payment and directory information
- Make sure provider records are current in the Provider Network Management (PNM) module.
- Providers should review and update their information regularly in the PNM module. AmeriHealth Caritas Ohio suggests at least monthly to avoid any payment issues.
- Provider specialties should be updated and captured as well as primary locations.
- When making changes, AmeriHealth Caritas Ohio recommends that providers allow time for updates from the PNM to populate in the Provider Master File.
- ODM can take up to 14 business days to approve and send changes to MCOs.
- If you are having difficulties getting your claims to AmeriHealth Caritas Ohio through the Fiscal Intermediary (FI), contact the Integrated Helpdesk at ODM 1-800-686-1516 or at IHD@Medicaid.ohio.gov.
- Providers can always request a reconciliation roster from their Provider Services Account Executive to make sure that data is being correctly reflected within our system and directories.
- Review panel changes, or your ability to accept new patients with your account representative to reduce patient abrasion.
Questions
If you have questions, please contact your Provider Account Executive or the Provider Services department at 1-833-644-6001.
|
|
NaviNet® care gap response workflow redesign
Currently, supplemental clinical documentation to close Care Gaps can be uploaded one member, one care gap at a time. The redesigned workflow will allow providers to resolve multiple Care Gaps in a specified group.
There are four major Care Gap groups included in this enhancement:
- Child and Adolescent Immunizations
- Care of Older Adults
- Transition of care
- Well-care visits
Upon accessing the Care Gap Response Form providers will notice two new columns have been added at the beginning of the form:
- Grouping Allowed? – Indicates which Care Gaps can be grouped together.
-
Rows can be grouped together for document upload/Care Gap closure if they share the same color icon, same Care Gap Group Name, and have a Provider Response Status of 'Response required.'
- Care Gap Group – Indicates the name of the Care Gap/HEDIS measure.
Providers will be able to select multiple Care Gaps in a grouping, upload supporting documents, and resolve the Care Gaps in the group.
Providers will also be able to access a new Member Roster page via a link on the Care Gap Response Form, instead of going back to Report Inquiry to pull a listing of all members with unresolved care gaps.
There will be no changes to the document types, upload size limits, and the ability to attach multiple documents.
NaviNet® disputes status enhancement
Providers can now view the status and a copy of the determination letter for previously submitted disputes via the NaviNet provider portal by accessing
Forms and Dashboards and selecting the Check Dispute Status link.
Search by one of the following data elements:
- Claim ID
- Member's ID
- Submission Date Range - Begin Date and End Date
Providers will be able to view 18 months of status history based on the dispute received date.
The search will return one of the following statuses:
In Progress, Approved, Rejected, Denied or
Voided and will include the date the determination letter was uploaded into the system. A copy of the determination letter will be available under Practice Documents.
This enhancement is designed to streamline your workflow by eliminating the need to:
- Call the health plan to obtain the status of your request.
- Wait to receive the determination letter by mail.
New to NaviNet?
If you do not have access to the NaviNet provider portal, please visit: https://register.navinet.net/ to sign up.
Questions
If you have questions or need further assistance, please contact your Provider Network Account Executive.
|
|
|---|
|
 Prior authorizations Prior authorizations |
|
|---|
|
Prior authorization removal effective Jan. 1
Beginning on January 1, prior authorization for the HCPCS codes and services listed in the table do not require prior authorization for in-network or out-of-network providers.
Did you know?
- You can submit prior authorization requests on our secure provider portal NaviNet, and in some instances receive auto-approval. Turnaround times are faster when using NaviNet.
- In the event you are unable to request a prior authorization, you can request a retro authorization if there is no claim on file. If no claim is on file, UM will review retro requests. Please contact your dedicated Account Executive with questions.
Out of network providers
Contact Utilization Management for prior authorization before providing care to our members: 1-833-735-7700. If you are interested in joining our network, contact our contracting department: providerrecruitmentoh@amerihealthcaritasoh.com. This email address can also be used by vision providers looking for in-network vendors who can provide eyeglass frames and lenses.
Submit all medical pharmacy prior authorizations (PA) to PerformRx
Prior authorization requests for prescriber administered medications should be submitted to PerformRx via fax. See our website for more information and the form.
|
|
 For behavioral health providers For behavioral health providers |
|
|---|
|
AmeriHealth Caritas Ohio is offering FREE training with pre-approved CEUs
The presentation will help clinicians understand key principles of Motivational Interviewing (MI) and applications for substance use disorders. Learners will have an opportunity to practice important skills associated with MI and will be pointed toward resources to help develop their MI practice.
- Introduction to Motivational Interviewing for Substance Use Disorders
- Virtually on Tuesday, Feb. 24, 1-2:30 p.m.
- 1.5 pre-approved CEUs for Ohio counselors, social workers, and marriage and family therapists.
|
|
|---|
|
Upcoming changes to eligibility for OhioRISE members
The Ohio Department of Medicaid intends to amend the OhioRISE: eligibility and enrollment rule, 5160-59-02, so that enrollment in OhioRISE will become effective the first day of the calendar month of eligibility. This change is being made to align with managed care program enrollment and to reduce manual retro-enrollments due to an inpatient behavioral health admission. The rule change is intended to be effective July 1.
Clarification of financial responsibility for behavioral health services provided to children and youth is found in the OhioRISE Mixed Services Protocol (Protocol). Managed care plans will still be responsible for CANS assessments completed prior to OhioRISE enrollment. The Protocol will be updated as needed to support the rule change.
This change in retro eligibility to the first day of calendar month that a member becomes eligible for OhioRISE may cause behavioral health claims that paid to be taken back so that the claim can be resubmitted to the OhioRISE plan for processing.
|
|
|---|
|
Billing reminder - rendering practitioners/affiliation
ODM requires that the rendering practitioner for behavioral health services be listed on claims submitted to Ohio Medicaid for payment. Their personal National Provider Identifier (NPI) must be reported in the rendering field on the claim for each service they provide. All rendering practitioners are required to have an NPI to render services to Medicaid enrollees AND they will be required to enroll in the Ohio Medicaid program and affiliate with their employing/contracting agency. Information about obtaining an NPI is available at: https://nppes.cms.hhs.gov/login. Once the rendering practitioner has obtained an NPI, they must enroll as a provider in the Ohio Medicaid Program via the Provider Network Management (PNM) portal. More details on this process are available at: https://managedcare.medicaid.ohio.gov/managed-care/centralized-credentialing/about-pnm.
CEU opportunities
Sign up to receive email about upcoming AmeriHealth Caritas Ohio’s free Continuing Education Unit (CEU) opportunities.
Submitting prior authorization (PA) requests for behavioral health services
See the tip sheet for guidance on submitting PAs for behavioral health service requests. |
|
|---|
|
 Resources and reminders Resources and reminders |
|
|---|
|
PCP change form
Do you have a patient whose Member ID card does not have you listed as their assigned PCP? You can use this PCP change form to request the members PCP be changed. Access the form here.
Multi-factor authentication for Care Coordination Portal access
To increase protection for the Managed Care Organization Care Coordination Portal’s and member information data, signing in will soon require Multi-Factor Authentication (MFA). MFA is a two-factor authentication process that takes user verification a step beyond the State of Ohio (OHID) and password. This is done by using a second source of validation (i.e., text message, email, passkey, phone call) to verify user identity before granting access.
HEDIS guidelines for the Care Gap Closure program
The HEDIS 2025 Documentation and Coding Guidelines for care delivered in 2025 can be viewed at NaviNet.
|
|
 Training opportunities Training opportunities |
|
|---|
|
Virtual office hours
Got Questions? Let us help you. Join the AmeriHealth Caritas Ohio Provider Services team for a virtual office hour. Our team will be here to help answer your questions or help you navigate our provider resources. No registration is necessary. Just click here to join.
Tuesday, Jan. 27
Noon to 1 p.m.
Value-based Reimbursement |
|
|---|
|
Cultural competency training opportunities
AmeriHealth Caritas Ohio is committed to promoting education and awareness of culturally and linguistically appropriate services (CLAS) and to combatting the effects of low health literacy on the health status of our members. |
|
|---|
|
Sign up for this newsletter
Our monthly newsletter, Provider Partnerships, keeps you informed about plan news, updates, and resources. Click here to sign up.
|
|
|---|
|
Need help?
AmeriHealth Caritas Ohio Provider Services is ready to help.
|
|
|---|
|
|
|
|
|  |
|
|
|
|
