|
|
|
Help us improve care – your voice matters and you’ll be entered to win new Apple AirPods Pro 3 for taking our survey! |
|
|---|
|
We value your expertise and want to hear from you. As part of our Voice of the Customer campaign, we’re asking medical providers like you to share feedback on closing gaps in care.
Your input will help us better support your practice and improve patient outcomes. The survey takes less than 5 minutes, and your insights will make a real difference.
And as a thank you, if you complete the survey by 1/9/26 you will be entered into a drawing on 1/12/26 to win Apple AirPods Pro 3 (valued at $249).
Click here to start the survey. |
|
|
Want to earn even more?
The holiday season is here and we'd like to gift you more chances to earn MORE money for the New Year!
Please be on the lookout as your Account Executive will be communicating another opportunity to earn money for closing even more gaps in care. In the next couple of weeks, we will be debuting a new incentive plan to close Breast Cancer Screening (BCS) and Colorectal Cancer Screenings (COL) through a multi-year look back. This opportunity is only being offered to a limited number of providers, and you are one of them!
Thank you for partnering with us to enhance care quality and performance.
|
|
|---|
|
Updated COVID-19 vaccine guidelines for 2025
The Food and Drug Administration (FDA) has updated the approvals and eligibility criteria for COVID-19 vaccines.
AmeriHealth Caritas Ohio covers the COVID-19 vaccine at no cost for members of all ages (age limits for children vary by manufacturer) when the vaccine is administered in a primary care provider’s (PCP) office or through a participating pharmacy.
For more information and a list of medical conditions that place individuals at a higher risk of severe illness, please go to www.cdc.gov/covid/risk-factors.
Please note: The medical condition list does not include all medical conditions that place a person at higher risk of severe illness from COVID-19. Rare medical conditions, including many conditions that mostly affect children, may not be included on this list.
A person with a condition that is not listed may still be at greater risk than other people of getting very sick from COVID-19.
|
|
|
As vaccine guidance continues to develop, we encourage our members to seek recommendations directly from you, their PCP. Thank you for staying informed during this evolving time and for your ongoing commitment to the health of those we serve.
Virtual autism assessments
AmeriHealth Caritas Ohio has partnered with the Zest Pediatric Network to offer virtual autism evaluations from specially trained pediatricians using standardized assessment tools. This will allow AmeriHealth Caritas Ohio members throughout the state to get appointments within weeks instead of months and complete the assessments from the comfort of their own homes. If the child is between 18 months and 11 years old and has shown signs of a developmental delay or autism spectrum disorder, or is currently on a waitlist for evaluation, the Zest Pediatric Network will help with the next steps. More information can be found here.
|
|
|---|
|
Help us support our members by sharing data
In support of our commitment to equitable healthcare access and improved provider and patient relations, we invite our providers to voluntarily share their demographic information. This includes your race and the languages you, and your practices speak.
This data helps us better reflect the diversity of our networks, support member choice, and helps improve access to culturally responsive care.
Our members value the ability to connect with providers who understand their cultural and linguistic preferences.
By collecting race, ethnicity, and language (REL) data we can:
- Highlight the diversity of our provider network.
- Improve how we present provider information.
- Support compliance with national standards including but not limited to Cultural Linguistic Appropriate Services (CLAS) and National Committee for Quality Assurance (NCQA) Accreditation.
AmeriHealth Caritas Ohio collects provider REL data through our standard processes, including credentialing, re-credentialing, and provider roster updates, using the federal categories established by the Office of Management and Budget (OMB).
REL data is housed in a database that is made available to members.
- Gender data, provider and staff languages, and additional language services are available through AmeriHealth Caritas Ohio provider directory.
- Race and ethnicity information are not displayed in the provider directory. The information is only made available to members upon request.
If you have questions, please contact your Provider Account Executive or the Provider Services department at 1-833-644-6001.
Thank you for partnering with us in advancing health equity. |
|
Ohio Department of Medicaid (ODM) updates
To stay up to date on ODM news, subscribe to the ODM Press.
Billing codes
ODM has provided guidance on billing codes for multiple births through Medicaid Advisory Letter (MAL) No. 685. This MAL can be found here.
With the new integrated Ohio Medicaid Enterprise System (OMES), delivery codes for multiple births should be reported on separate details on the claim with modifier 51 appended.
Modifiers
The Modifiers Recognized by Ohio Medicaid Fee-For-Service document has been updated. Have questions on what the correct modifier is to use for a service or supply procedure? ODM’s website has a list of approved modifiers.
Tips for contacting the Ohio Medicaid Integrated Helpdesk
The Integrated Helpdesk (IHD) is a great resource to use when you run into an issue. It provides 24-hour, seven days a week access to information regarding client eligibility, claim and payment status, and provider information. Call 1-800-686-1516 or email IHD@medicaid.ohio.gov.
Provider education and training resources
It is important that providers update all 1099 address information in the Provider Network Management (PNM) module regularly. Ensure all information is current, including extra address details like suite number, house/office number, etc. to reduce the chance of non-delivery by the postal service. Access the quick reference guides here.
|
|
|---|
|
Ohio Department of Medicaid email links
|
|
|---|
|
 Claims and billing Claims and billing |
|
|---|
|
Questions about reimbursement or payment policies?
Click the appropriate link below for more detailed information.
Clinical Policies
Electronic claims submission
Providers can choose the submission option that works for them. It can be any approved clearinghouse or direct to ODM. Preferred options are:
- Availity (subscription)
- Change Healthcare (no cost)
Claim attachments
Step 1: Go to Availity attachment portal, send the attachments first. Make sure the “Attachment Control #” is unique to that claim and make note of it. For example, if they are sending three attachments then, Attachment A – 111111, Attachment B – 22222, …
Step 2: Go to Change Healthcare's portal, ConnectCenter. When keying in the claim, in the attachment section, add the “Attachment Control #” which they noted (111111, 222222, ...). And from the drop-down menu choose the right “Attachment type.”
Note: “Attachment Control #” must be unique for that claim. You can add Member name or anything, but it must be unique for that claim. In other words, you can use 111111, 222222, … for the second claim you are submitting.
NaviNet pro tips
Claims Investigations
- If a provider has multiple offices or TINs, users must be linked to each TIN for the corresponding office to view claims and remittance advice.
- In a claims investigation, only certain documents are permitted to be uploaded to the investigation function. If the document type is not listed below, a dispute must be filed, and the document should be attached with the dispute.
- EOBs should not be uploaded for COB when a claim denies for “EOB from primary payer required.” Please send a corrected claim or file a dispute. EOBs for non-covered or exhausted benefits letters are permitted to be uploaded in the investigation.
How to file a Dispute in NaviNet
Electronic funds transfer
AmeriHealth Caritas Ohio has contracted with Change Healthcare and ECHO® Health, Inc., to administer electronic funds transfer (EFT) payments. There are no fees for single payer agreements to receive a direct payment from AmeriHealth Caritas Ohio via EFT or to receive an electronic remittance advice (ERA). Click to learn how to enroll, the payment schedule, and more.
Claims Payment Systemic Error report
The Claims Payment Systemic Errors (CPSE) report is updated and posted monthly on our website. AmeriHealth Caritas Ohio encourages you to review this log frequently and before contacting our Provider Services team. If you have additional questions, please reach out to Provider Services at 1-833-644-6001 and, as always, you can reach out to your local account executive.
Dispute or appeal?
If a provider disagrees with the outcome of a claim, the first step should always be to submit a claim dispute.
Provider disputes
Provider claim disputes are any provider inquiries or requests for reconsiderations, ranging from general questions about a claim to a provider disagreeing with a claim denial. Provider Dispute Submission Form (PDF)
A dispute can be submitted using any of the following methods:
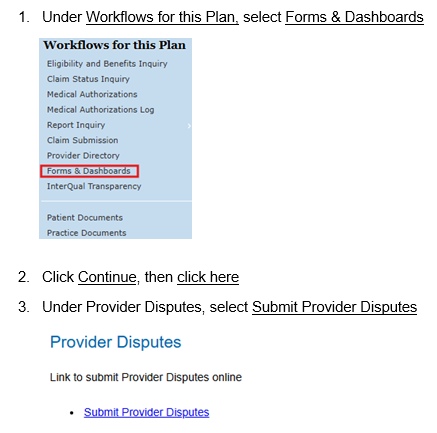
- NaviNet (recommended method): Providers can submit a dispute with attachments to AmeriHealth Caritas Ohio via NaviNet instead of faxing or mailing. Log in, go to Forms & Dashboards, scroll down to Provider Disputes, click the Submit Provider Disputes link. The turnaround time is 15 days for disputes.
- Mail the form with your supporting documentation to:
AmeriHealth Caritas Ohio
Attn: Provider Claim Inquiry
P.O. Box 7126
London, KY 40742
- Phone: 1-833-644-6001. Select the prompts for the correct department and then select the prompt for claim issues.
- Fax: 1-833-216-2272
Provider appeals
Providers may file an appeal on a denied pre-service within 30 days of the notice of Adverse Benefit Determination (ABD).
- Mail the form with your supporting documentation to:
AmeriHealth Caritas Ohio
Attn: Provider Claim Inquiry
P.O. Box 7400
London, KY 40742
- Fax: 1-833-564-1329
Best practices to ensure accurate payment and directory information
- Make sure provider records are current in the Provider Network Management (PNM) module.
- Providers should review and update their information regularly in the PNM module. AmeriHealth Caritas Ohio suggests at least monthly to avoid any payment issues.
- Provider specialties should be updated and captured as well as primary locations.
- When making changes, AmeriHealth Caritas Ohio recommends that providers allow time for updates from the PNM to populate in the Provider Master File.
- ODM can take up to 14 business days to approve and send changes to MCOs.
- If you are having difficulties getting your claims to AmeriHealth Caritas Ohio through the Fiscal Intermediary (FI), contact the Integrated Helpdesk at ODM 1-800-686-1516 or at IHD@Medicaid.ohio.gov.
- Providers can always request a reconciliation roster from their Provider Services Account Executive to make sure that data is being correctly reflected within our system and directories.
- Review panel changes, or your ability to accept new patients with your account representative to reduce patient abrasion.
Questions
If you have questions, please contact your Provider Account Executive or the Provider Services department at 1-833-644-6001.
|
|
NaviNet® care gap response workflow redesign
Currently, supplemental clinical documentation to close Care Gaps can be uploaded one member, one care gap at a time. The redesigned workflow will allow providers to resolve multiple Care Gaps in a specified group.
There are four major Care Gap groups included in this enhancement:
- Child and Adolescent Immunizations
- Care of Older Adults
- Transition of care
- Well care visits
Upon accessing the Care Gap Response Form providers will notice two new columns have been added at the beginning of the form:
- Grouping Allowed? – Indicates which Care Gaps can be grouped together.
-
Rows can be grouped together for document upload/Care Gap closure if they share the same color icon, same Care Gap Group Name, and have a Provider Response Status of 'Response required.'
- Care Gap Group – Indicates the name of the Care Gap/HEDIS measure.
Providers will be able to select multiple Care Gaps in a grouping, upload supporting documents, and resolve the Care Gaps in the group.
Providers will also be able to access a new Member Roster page via a link on the Care Gap Response Form, instead of going back to Report Inquiry to pull a listing of all members with unresolved care gaps.
There will be no changes to the document types, upload size limits, and the ability to attach multiple documents.
NaviNet® disputes status enhancement
Providers can now view the status and a copy of the determination letter for previously submitted disputes via the NaviNet provider portal by accessing
Forms and Dashboards and selecting the Check Dispute Status link.
Search by one of the following data elements:
- Claim ID
- Member's ID
- Submission Date Range - Begin Date and End Date
Providers will be able to view 18 months of status history based on the dispute received date.
The search will return one of the following statuses:
In Progress, Approved, Rejected, Denied or
Voided and will include the date the determination letter was uploaded into the system. A copy of the determination letter will be available under Practice Documents.
This enhancement is designed to streamline your workflow by eliminating the need to:
- Call the health plan to obtain the status of your request.
- Wait to receive the determination letter by mail.
New to NaviNet?
If you do not have access to the NaviNet provider portal, please visit: https://register.navinet.net/ to sign up.
Questions
If you have questions or need further assistance, please contact your Provider Network Account Executive.
|
|
|---|
|
📰 Understanding balance billing in Medicaid
As a contracted provider with AmeriHealth Caritas Ohio, it’s essential to understand the rules and responsibilities around balance billing to ensure compliance and protect our Medicaid members.
🚫 When billing a Medicaid member is not permitted
Providers may not bill Medicaid recipients when a claim is denied due to:
- Unacceptable or untimely claim submission
- Failure to obtain prior authorization
- Retroactive determination by a Peer Review Organization (PRO) that the service was not medically necessary
These denials do not transfer financial responsibility to the member.
✅ When billing may be permitted
A provider may bill a Medicaid recipient in lieu of submitting a claim to the Ohio Department of Medicaid (ODM) only if all of the following conditions are met:
- The provider informs the member that the service is covered by Medicaid and that other providers may offer it at no cost.
- The provider notifies the member in writing—before each date of service—that they will not submit a claim to ODM.
- The member signs a written agreement acknowledging financial responsibility before the service is rendered.
- The service is not a prescription for a controlled substance as defined in Ohio Revised Code §3719.01.
Additionally, non-covered services (including those denied for lack of prior authorization) may be billed to the member only if the written notification and agreement steps above are followed.
💡 Important reminder
Under the Social Security Act, all payments from AmeriHealth Caritas Ohio to participating providers must be accepted as payment in full. Members may not be balance billed for medically necessary covered services under any circumstance.
📌 What this means for you
Balance billing violations can result in compliance actions and member grievances. Please ensure your billing practices align with ODM and AmeriHealth Caritas Ohio policies. If you have questions, contact your Provider Relations representative.
|
|
|---|
|
 Prior authorizations Prior authorizations |
|
|---|
|
Did you know?
- You can submit prior authorization requests on our secure provider portal NaviNet, and in some instances receive auto-approval. Turnaround times are faster when using NaviNet.
- In the event you are unable to request a prior authorization, you can request a retro authorization if there is no claim on file. If no claim is on file, UM will review retro requests. Please contact your dedicated Account Executive with questions.
Out of network providers
Contact Utilization Management for prior authorization before providing care to our members: 1-833-735-7700. If you are interested in joining our network, contact our contracting department: providerrecruitmentoh@amerihealthcaritasoh.com. This email address can also be used by vision providers looking for in-network vendors who can provide eyeglass frames and lenses.
Submit all medical pharmacy prior authorizations (PA) to PerformRx
Prior authorization requests for prescriber administered medications should be submitted to PerformRx via fax. See our website for more information and the form.
|
|
 For behavioral health providers For behavioral health providers |
|
|---|
|
AmeriHealth Caritas Ohio is offering FREE training with pre-approved CEUs
The presentation will help clinicians understand key principles of Motivational Interviewing (MI) and applications for substance use disorders. Learners will have an opportunity to practice important skills associated with MI and will be pointed toward resources to help develop their MI practice.
- Introduction to Motivational Interviewing for Substance Use Disorders
- Tuesday, Feb. 24, 2026, 1-2:30 p.m.
- 1.5 pre-approved CEUs for Ohio counselors, social workers, and marriage and family therapists.
|
|
|---|
|
Billing reminder - rendering practitioners/affiliation
ODM requires that the rendering practitioner for behavioral health services be listed on claims submitted to Ohio Medicaid for payment. Their personal National Provider Identifier (NPI) must be reported in the rendering field on the claim for each service they provide. All rendering practitioners are required to have an NPI to render services to Medicaid enrollees AND they will be required to enroll in the Ohio Medicaid program and affiliate with their employing/contracting agency. Information about obtaining an NPI is available at: https://nppes.cms.hhs.gov/login. Once the rendering practitioner has obtained an NPI, they must enroll as a provider in the Ohio Medicaid Program via the Provider Network Management (PNM) portal. More details on this process are available at:https://managedcare.medicaid.ohio.gov/managed-care/centralized-credentialing/about-pnm.
CEU opportunities
Sign up to receive email about AmeriHealth Caritas Ohio’s free Continuing Education Unit (CEU) opportunities.
Submitting prior authorization (PA) requests for behavioral health services
See the tip sheet for guidance on submitting PAs for behavioral health service requests. |
|
|---|
|
 Resources and reminders Resources and reminders |
|
|---|
|
PCP change form
Do you have a patient whose Member ID card does not have you listed as their assigned PCP? You can use this PCP change form to request the members PCP be changed. Access the form here.
Multi-factor authentication for Care Coordination Portal access
To increase protection for the Managed Care Organization Care Coordination Portal’s and member information data, signing in will soon require Multi-Factor Authentication (MFA). MFA is a two-factor authentication process that takes user verification a step beyond the State of Ohio (OHID) and password. This is done by using a second source of validation (i.e., text message, email, passkey, phone call) to verify user identity before granting access.
HEDIS guidelines for the Care Gap Closure program
The HEDIS 2025 Documentation and Coding Guidelines for care delivered in 2025 can be viewed at NaviNet.
|
|
 Training opportunities Training opportunities |
|
|---|
|
Virtual office hours
Got Questions? Let us help you. Join the AmeriHealth Caritas Ohio Provider Services team for a virtual office hour. Our team will be here to help answer your questions or help you navigate our provider resources. No registration is necessary. Just click here to join.
Tuesday, Jan. 27, 2026
Noon to 1 p.m.
Value-based Reimbursement |
|
|---|
|
Cultural competency training opportunities
AmeriHealth Caritas Ohio is committed to promoting education and awareness of culturally and linguistically appropriate services (CLAS) and to combatting the effects of low health literacy on the health status of our members. |
|
|---|
|
Tell us a little bit about where you’re from and where you went to school.
I grew up in Cleveland, Ohio, and attended John Hay Hough School and Dyke College.
Everyone at AmeriHealth Caritas Ohio has a story about why they joined the team. What’s yours?
I joined the team after a conversation with Mike Hibbard, a former colleague from another managed care plan. The opportunity was ideal because I had been working in Corporate Communications and knew I could make a meaningful impact on AmeriHealth Caritas Ohio’s Member Engagement–Community Outreach Team.
What drew you to this profession?
My introduction to healthcare began on the corporate side of the business, and I wanted the chance to experience the industry from a different perspective.
If you could have dinner with anyone in the world, dead or alive, who would it be? Why?
If I could have dinner with anyone, it would be both of my grandmothers. They passed away years ago, but I deeply miss the conversations we shared.
What do you like to do in your free time?
In my free time, I am an avid tennis player and a member of the Forest City Tennis Club, one of the oldest African American tennis organizations in the United States.
|
|
|
What are 2 apps on your phone you CANNOT live without?
Facebook and Pandora.
Any interesting facts about yourself that you’d like to share?
I began working at the Cleveland Trust Bank at age 15 and expected to build a long-term career in banking, until my time at Kaiser Permanente introduced me to an entirely new path. I have been in healthcare ever since!
|
|
|---|
|
Give the Gift of Sight Month
According to the CDC, only half of the estimated 93 million American adults at a higher risk for vision loss have had an eye exam in the past year. Half of all blindness is preventable when eye diseases are diagnosed in the early stages. Give the Gift of Sight Month serves as an annual reminder to get your eye exam so you can have visions of twinkling lights and sugar plum fairies for years to come! You can also participate in this observance by supporting non-profits that provide free glasses or eye exams or recycling your frames. |
|
|
|
|
Sign up for this newsletter
Our monthly newsletter, Provider Partnerships, keeps you informed about plan news, updates, and resources. Click here to sign up.
|
|
|---|
|
Need help?
AmeriHealth Caritas Ohio Provider Services is ready to help.
|
|
|---|
|
|
|
|
|  |
|
|
|
|
