|
|
|
|
|
|
Provider Services 1-833-644-6001 |
|
|---|
|
|
About the Provider Master File
In an effort to better serve our provider network, AmeriHealth Caritas Ohio has accepted rosters from providers as an additional level of validation against the Provider Master File (PMF) data.
Since the Source of Truth launch in October 2023, AmeriHealth Caritas Ohio has been monitoring its network providers and their utilization of the PMF. It has been noted the majority of providers are now maintaining their records through the source of truth.
Beginning July 1, AmeriHealth Caritas Ohio will cease all reconciliation efforts using rosters unless contractually obligated to do so. We encourage all providers to update their information in the PNM to ensure the most up to date information.
Best practices to ensure accurate payment and directory information
- Make sure provider records are current in Provider Network Management (PNM) module.
- Providers should review and update their information regularly in the PNM. AmeriHealth Caritas Ohio suggests at least monthly to avoid any payment issues.
- Provider specialties should be updated and captured as well as primary locations.
- When making changes, AmeriHealth Caritas Ohio recommends that providers allow time for updates from the PNM to populate in the Provider Master File.
- ODM can take up to 14 business days to approve and send changes to MCOs.
- If you are having difficulties getting your claims to AmeriHealth Caritas Ohio through the Fiscal Intermediary (FI) contact the Integrated Helpdesk at ODM 1-800-686-1516 or at IHD@Medicaid.ohio.gov.
- Providers can always request a reconciliation roster from their Provider Services Account Executive to make sure that data is being correctly reflected within our system and directories.
- Review panel changes, or your ability to accept new patients with your account representative to reduce patient abrasion.
|
|
Measles cases are rising: help us protect our members
As you may be aware, measles outbreaks have been reported in several states, including Ohio, with increased case counts in both urban and rural areas. Most of these cases were among children and adolescents who had not received a measles vaccine or whose vaccination history is unknown. Populations most at-risk of serious complications if infected include infants, young children, pregnant individuals, and persons with compromised immune systems. The CDC has issued alerts reminding healthcare providers to remain vigilant, particularly in communities with low MMR vaccination coverage.
Measles is extremely contagious.
- It begins with fever, cough, coryza (runny nose), and conjunctivitis (pink eye).
- Followed 2–4 days later by a rash that starts on the face and spreads downward on the body.
- Infected people are contagious from four days before the rash starts through four days afterward.
- The virus is transmitted by direct contact with infectious droplets or by airborne spread when an infected person breathes, coughs, or sneezes and can remain infectious in the air and on surfaces for up to two hours after an infected person leaves an area.
- Measles can cause severe health complications, including pneumonia, encephalitis, and death.
The Measles, Mumps, and Rubella (MMR) vaccination remains the best way to protect against measles and its complications.
Click for CDC measles vaccine recommendations
As trusted partners in care, you play a vital role in reviewing immunization records at every visit, educating patients about the benefits and safety of vaccines, and recommending the MMR vaccine clearly and confidently to hesitant members and families. We encourage you to leverage every patient interaction—especially well-child visits, postpartum check-ins, and back-to-school appointments—to check and update vaccination status.
Additional resources
|
|
|---|
|
Reducing disparities in the management of hypertension in African American members |
|
|---|
|
We are pleased to announce the launch of AmeriHealth Caritas Ohio’s toolkit titled Reducing Disparities in the Management of Hypertension in African American Patients. This toolkit covers topics such as barriers to care within the African American population and supportive best practices, tools, and strategies when working to reduce high blood pressure for your African American patient population.
This toolkit will provide you with access to culturally responsive best practices
|
|
|
when providing care to African American patients with hypertension. We hope that you find this toolkit useful when providing care to your patients.
|
|
|---|
|
New Home Health Aide training program
To support meaningful employment for Medicaid enrollees, AmeriHealth Caritas Ohio has launched a new benefit for plan members, the Home Health Aide (HHA) Training Program. Administered by the Ohio Council for Home Care & Hospice. The program provides cost-free training and certification to AmeriHealth Caritas Ohio members seeking to become employed as an HHA. This new member benefit promotes and supports meaningful employment opportunities for Medicaid enrollees and addresses the need for more home health aides in Ohio.
AmeriHealth Caritas Ohio is seeking home health agency partners to support a member’s successful completion of this program. Specifically, the home health agencies would be responsible to administer an exam and facilitate a skills assessment.
Partner with us today to increase your pool of eligible HHAs that meet both CMS and PASSPORT requirements!
Contact Carmen Clutter, Director, Population Health Management for additional details.
|
|
|---|
|
Electronic Visit Verification - warning codes are live!
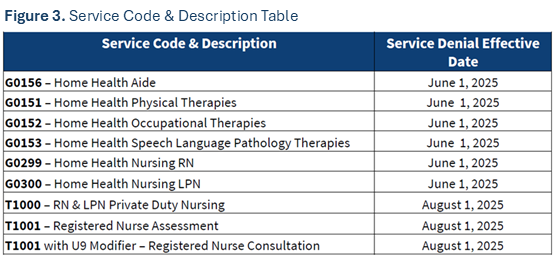
Providers began seeing warning codes on their remittance advice statements in April. As a reminder, providers will begin to see warning codes transition to hard denials on June 1.
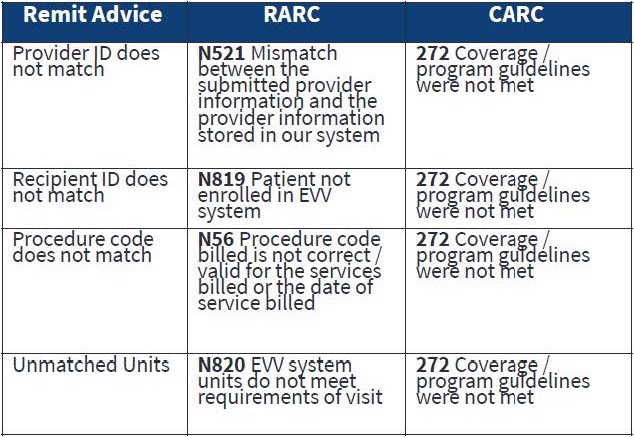
Please note the services and provider types that are subject to Electronic Visit Verification and the corresponding implementation phases. All providers must comply with ODM policy around verification, or they could experience denials beginning June 1.
|
|
We want to hear from you!
AmeriHealth Caritas Ohio wants to ensure we are providing you with the best service as you care for your patients, our members. We have developed a very short survey and would greatly appreciate it if you would complete it. This will allow us to better understand our opportunities for improvement.
Thank you in advance for participating! |
|
|
|
|---|
|
Ohio Department of Medicaid (ODM) updates
To stay up to date on ODM news, subscribe to the ODM Press.
ODM to roll out EVV claims processing changes in seven phases
The Ohio Department of Medicaid has begun the roll out of Electronic Visit Verification
(EVV) claims validation requirements for home health services that are billed to Ohio Medicaid to ensure claims requiring electronic visit verification have a matching EVV visit record upon submission. Claims that do not match will be denied.
A list of services and their execution dates, and a claims validation process flowchart can be found on ODM's website.
Tips for contacting the Ohio Medicaid Integrated Helpdesk
The Integrated Helpdesk (IHD) is a great resource to use when you run into an issue. It provides 24 hour, seven days a week access to information regarding client eligibility, claim and payment status, and provider information. Read the useful tips here.
Important reminder: Update 1099 address information in the Provider Network Management module
It is important that providers update all 1099 address information in the Provider Network Management (PNM) module regularly. Ensure all information is current, including extra address details like suite number, house/office number, etc. to reduce the chance of non-delivery by the postal service. Access the quick reference guides here.
New features implemented in the Ohio Medicaid Enterprise System
The New Features Implementation Overview outlines key changes for providers.
Medicaid agreement revalidations
To complete revalidation, visit PNM & Centralized Credentialing.
Ohio Department of Medicaid fraud warning
If your Medicaid patient is contacted for their personal information, advise them not to respond. Report it to the Ohio Attorney General at 1-800-282-0515 or via the online form.
Updated claim submission and adjudication FAQ
Claims and Prior Authorization Submission Frequently Asked Questions (FAQ)
|
|
|---|
|
Ohio Department of Medicaid email links
|
|
|---|
|
 Claims and billing Claims and billing |
|
|---|
|
New functionality - NaviNet® claims investigation attachments
AmeriHealth Caritas Ohio and NantHealth|NaviNet are excited to announce that we are bringing you a new feature: Claim Investigation Attachments. You can now upload supporting documents with your electronic claim investigation request within the NaviNet provider portal!
This enhancement is designed to streamline your workflow by eliminating the need to complete forms and fax/mail supporting documentation
Each supporting document will need to be 32 MB or smaller and in one of the following formats:
New to Claim Investigations in NaviNet?
Once logged into the portal, view the Claims investigation training video for a walk-through of the process.
New to NaviNet?
If you do not have access to the NaviNet provider portal, please visit: https://register.navinet.net/ to sign up.
If you have questions or need further assistance, contact the NaviNet Customer Support team at 1-888-482-8057, Monday through Friday, 8 a.m. to 11 p.m.
Electronic data interchange
Providers with electronic data interchange (EDI) capabilities may submit claims, eligibility inquiries, claim status inquiries, and associated attachments by being a trading partner authorized by ODM or by contracting with an ODM-authorized trading partner. For more information, visit the ODM trading partners webpage or call the ODM IHD at 1-800-686-1516.
Direct Data Entry
For Direct Data Entry (DDE), providers should log in to Change Healthcare using the tool called ConnectCenter to improve claims management functionality. Providers who have a limited ability to submit claims through their hospital or project management system may now benefit from key features of the ConnectCenter tool. There is no cost to providers to use ConnectCenter. Learn more on our claims and billing webpage.
Connectivity restored with Optum/Change Healthcare
The restoration of connectivity with Optum/Change Healthcare gives our providers options for claims submissions. Click here to learn more about the electronic and manual/direct entry options.
Questions about reimbursement or payment policies?
Click the appropriate link below for detailed information.
No paper claims
The Next Generation of Ohio Medicaid program's guidelines require all claims to be submitted via the Electronic Data Exchange (EDI). Use AmeriHealth Caritas Ohio’s EDI Payer ID# 35374. You can get started on our website with claims how-tos, quick guides, links, and contact info.
Claims Payment Systemic Error report
The Claims Payment Systemic Errors (CPSE) report is updated and posted monthly on our website. AmeriHealth Caritas Ohio encourages you to review this log frequently and before contacting our Provider Services team. If you have additional questions, please reach out to Provider Services at 1-833-644-6001 and, as always, you can reach out to your local account executive.
Submitting claim disputes on NaviNet
If a provider disagrees with the outcome of a claim, the first step should always be to submit a claim dispute via fax or online. Below are the steps to submit a claim dispute on our NaviNet portal:
Although the dispute is being submitted online, all resulting correspondence will still be received via mail.
Providers can submit a dispute with attachments to AmeriHealth Caritas Ohio via NaviNet. Providers have the option to submit disputes through NaviNet, instead of faxing or mailing. We recommend providers use this option. Log into NaviNet, go to Forms & Dashboards, scroll down to Provider Disputes, then click on the Submit Provider Disputes link. Turnaround time is 15 days for disputes.
|
|
 Prior authorizations Prior authorizations |
|
|---|
|
Contact Utilization Management for a prior authorization before to providing care to our members: 1-833-735-7700. Additionally, if interested in joining our network please reach out to our Contracting department via email at: providerrecruitmentoh@amerihealthcaritasoh.com. This email address can also be used by vision providers looking for in-network vendors who can provide eyeglass frames and lenses.
Submit prior authorization requests (PA) electronically through NaviNet
AmeriHealth Caritas Ohio offers our providers access to our Medical Authorizations portal for electronic authorization inquiries and submission. The portal is accessed through NaviNet and located on the Workflows menu.
In addition to submitting and inquiring on existing authorizations, you will also be able to:
- Verify if no authorization is required
- Receive auto approvals, in some circumstances
- Submit amended authorization
- Attach supplemental documentation
- Sign up for in-app status change notifications directly from the health plan
- Access a multi-payer authorization log
- Submit inpatient concurrent reviews online if you have health information exchange (HIE) capabilities (fax is no longer required)
- Review inpatient admission notifications and provide supporting clinical documentation
Submit all medical pharmacy prior authorizations (PA) to PerformRx
Prior authorization requests for prescriber administered medications should be submitted to PerformRx via fax. See our website for more information and the form.
|
|
 For behavioral health providers For behavioral health providers |
|
|---|
|
Questions regarding The American Society of Addiction Medicine Criteria Fourth Edition, Volume 1 – Adults
- Does ODM have a date in mind for adopting the Fourth Edition Criteria into Ohio Medicaid coverage and reimbursement policies? Given the extent of the changes included in the Fourth Edition, Volume 1 – Adults, the Department will not establish a timeline for implementation until it has completed the review and stakeholder engagement processes.
- What criteria will the managed care entities use when rendering a decision on a prior authorization request? Medicaid managed care entities will use the Third Edition Criteria when rendering a decision on a prior authorization request for SUD services until ODM formally adopts use of the Fourth Edition Criteria, Volume 1 – Adults. If a provider chooses to move towards the adoption of the Fourth Edition criteria prior to the State’s adoption, the provider must ensure that a request for PA meets the Third Edition criteria.
CEU opportunities
Sign up to receive email about AmeriHealth Caritas Ohio’s free Continuing Education Unit (CEU) opportunities.
Submitting prior authorization (PA) requests for behavioral health services
See the tip sheet for guidance on submitting PAs for behavioral health service requests.
|
|
Bright Start® maternity program
Bright Start helps our members stay healthy when they are pregnant and have a healthy baby. Members get access to our pregnancy care program to help schedule appointments and connect to community resources and additional programs. Visit the links below to learn more about this valuable program for your pregnant patients.
Care for pregnant members
Bright Start Welcome Booklet
Bright Start Beginnings Bundle
|
|
|---|
|
We are now covering doula services
AmeriHealth Caritas Ohio is dedicated to improving health outcomes for pregnant Medicaid members. Any pregnant or postpartum person with Medicaid coverage is eligible to receive doula services from a Board of Nursing-certified, Medicaid-enrolled doula. Doulas have been shown to improve birth outcomes, support birth equity, positively impact the social determinants of health, and reduce disparities in maternal and infant outcomes.
Click here to read the coverage overview, visit types, and find resources.
To read the Ohio Medicaid Managed Care Organizations Consolidated Doula Resource Guide click here.
The Ohio Board of Nursing has released a new State of Ohio Certified Doula FAQs document, providing key information on certification requirements, scope of practice and other essential details for doulas in Ohio.
|
|
|---|
|
 Resources and reminders Resources and reminders |
|
|---|
|
Sign up for this newsletter
Our monthly newsletter, Provider Partnerships, keeps you informed about plan news, updates, and resources. Click here to sign up.
Member rights and responsibilities
AmeriHealth Caritas Ohio members have rights and responsibilities. We believe all members have the right to receive information on the services AmeriHealth Caritas must provide, the right to be treated with respect, dignity, and privacy.
- Members have the right to receive medically necessary treatment options for their conditions no matter the cost or benefit coverage
- Members are to take part in decisions about their healthcare.
- Members are to treat healthcare staff with respect, be aware of the benefits and services available to them.
- Ask for more explanations if they do not understand their doctors' instructions.
- To provide their physicians with accurate and complete medical information.
Redeterminations
We understand that many members may be unaware that their redetermination period is approaching, and your engagement can play a crucial role in ensuring they take the necessary steps to avoid a lapse in coverage. We encourage our providers to remind their patients that they may need to complete the redetermination process to help ensure they can retain their Medicaid benefits. Please let us know how we can support you in sharing this important information. We appreciate your partnership and commitment to member health and continuity of care.
Provider resources
We highly recommend providers take a few minutes to familiarize themselves with the tools available on our website. Our user-friendly tools and resources are designed to support Ohio’s Medicaid providers and your staff in giving members excellent and efficient healthcare.
- prior authorization lookup tool
- video tutorials for claims submission
- step-by-step instructions for claims submission and our secure provider portal NaviNet
- Provider Manual
- Provider Claims and Billing Manual
- contact information for our call center and AmeriHealth Caritas Ohio provider services
- monthly CPSE reports and trending claims issue information
Updated HEDIS guidelines for the Care Gap Closure program
View the HEDIS 2024 Documentation and Coding Guidelines for care delivered in 2024.
Provider Network Management (PNM) portal
Until it is fully active, please continue to send roster updates to both PNM and the MCO’s. Behavioral Health providers ARE able to only update through the PNM portal without submitting rosters to the MCO’s.
Credentialing reminder
Providers no longer need to complete credentialing with each managed care organization. Credentialing is now completed through the state's PNM portal. More information can be found here.
|
|
 Training opportunities Training opportunities |
|
|---|
|
New provider orientation schedule
Join us for virtual New Provider Orientation sessions. They are an opportunity for us to introduce AmeriHealth Caritas Ohio, how we operate, what tools and opportunities we have available to our providers, and what sets us apart from the other managed care organizations in the state. You can schedule an individual orientation for yourself or your staff with your account executive or can attend one of the virtual group sessions.
Your personal AmeriHealth Caritas Ohio Account Executives look forward to meeting you! Click here to see the entire calendar and register.
|
|
|---|
|
Comprehensive Primary Care (CPC) quarterly webinar series
The 2025 CPC quarterly webinar series will focus on keeping practices informed about the latest CPC updates, learning opportunities, discussions and more. Topics will be sent out ahead of time. Click here to register.
These take place from 9:30 a.m. to 11 a.m. on the following dates:
- Tuesday, September 16
- Tuesday, November 18
|
|
|---|
|
2025 CPC summer learning session registration is open
ODM will once again be hosting an in-person CPC Summer Learning Session for all currently enrolled CPC practices.
Dates: July 15 and July 22
Time: 9:30 a.m. to 3:30 p.m.
Where: 4200 Surface Road, Columbus, OH 43228
Room: Willow/Walnut conference room
This session is taking place twice to maximize attendance; however, the same information is being shared at both. If you plan on attending, please only register for one of the two dates.
We highly encourage at least one individual from all our CPC practices to attend. Space is limited so reserve your seat today!
|
|
|---|
|
Cultural competency training opportunities
AmeriHealth Caritas Ohio is committed to promoting education on and awareness of culturally and linguistically appropriate services (CLAS) and to combatting the effects of low health literacy on the health status of our members. |
|
|---|
|
Tell us a little bit about where you’re from and where you went to school.
I am originally from Northeast Pennsylvania near Scranton which is the home of The Office. I received my undergrad degree at Wilkes University and my MBA from Youngstown State.
Everyone at AmeriHealth Caritas Ohio has a story about why they joined the team. What’s yours?
We have always lived in Pennsylvania and since our daughter was graduating from high school, we decided it was time to try somewhere new. I was working for an MCO in PA, and I was looking for a similar role with a mission-driven organization that had strong ties to the community.
What drew you to this profession?
I started my career working in defined benefits, and health and welfare benefits for retirees. I discovered that I really |
|
|
enjoyed working with benefits and decided to change gears and went to work for a health insurance plan.
What do you like to do in your free time?
In my free time I like to work out, and we like to travel as a family. I also spend a lot of time watching my son play baseball and my daughter play lacrosse.
What are 2 apps on your phone you CANNOT live without?
Email and CrossFit app
Any interesting facts about yourself that you’d like to share?
I’ve never watched the movie Titanic.
|
|
|---|
|
Me and the family at a Phillies game. |
|
|---|
|
Did you know Mental Health Awareness Month has been observed in the U.S. since 1949? The purpose of Mental Health Month is to raise awareness and educate the public about mental illnesses and the realities of living with these conditions, as well as strategies for attaining mental health and wellness and reducing the stigma that surrounds mental illnesses.The 2025 theme is: Turn Awareness into Action. The Turn Awareness into Action theme was chosen with the goal of celebrating “the progress we’ve made in recognizing the importance of mental health- and challenging us to turn understanding into meaningful steps toward change.”
Check out the Mental Health Awareness Month Toolkit here.
|
|
|---|
|
Need help?
AmeriHealth Caritas Ohio Provider Services is ready to help.
|
|
|---|
|
|
|
|
|  |
|
|
|
|
