|
|
|
|
|
|
Provider Services 1-833-644-6001 |
|
|---|
|
|
2024 end-of-year provider incentive for adult well visits
AmeriHealth Caritas Ohio is pleased to announce that over 500 providers participated in our 2024 Quarter 4 Adult Well Visit Provider Incentive!
As a reminder, we offered a $50 incentive payment for each eligible adult Medicaid member seen for a comprehensive well visit between 10/1/2024 – 12/31/2024. This incentive was in addition to the standard reimbursement rate.
Providers can expect incentive payments (“bonus”) to disburse on/around April 17. Our providers’ commitment to delivering high-quality care for our members is truly commendable, and we are grateful for your partnership in promoting positive health outcomes through preventative care. Thank you! |
|
New Home Health Aide training program
To support meaningful employment for Medicaid enrollees, AmeriHealth Caritas Ohio has launched a new benefit for plan members, the Home Health Aide (HHA) Training Program. Administered by the Ohio Council for Home Care & Hospice. The program provides cost-free training and certification to AmeriHealth Caritas Ohio members seeking to become employed as an HHA. This new member benefit promotes and supports meaningful employment opportunities for Medicaid enrollees and addresses the need for more home health aides in Ohio.
AmeriHealth Caritas Ohio is seeking home health agency partners to support a member’s successful completion of this program. Specifically, the home health agencies would be responsible to administer an exam and facilitate a skills assessment.
Partner with us today to increase your pool of eligible HHAs that meet both CMS and PASSPORT requirements!
Contact Carmen Clutter, Director, Population Health Management for additional details.
|
|
|---|
|
Electronic Visit Verification - warning codes are live in April!
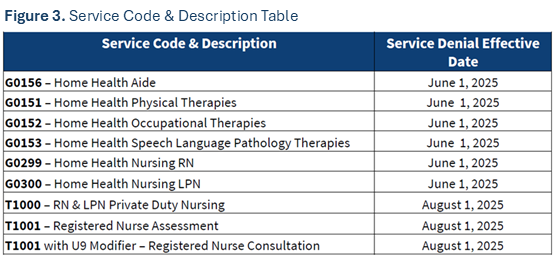
Providers will begin to see warning codes on their remittance advice statements this month. As a reminder, providers will begin to see warning codes transition to hard denials on June 1.
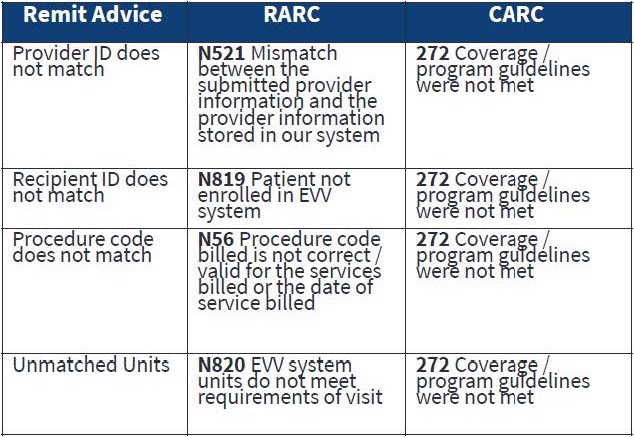
Please note the services and provider types that are subject to Electronic Visit Verification and the corresponding implementation phases. All providers must comply with ODM policy around verification or they could experience denials beginning June 1.
|
|
Ohio Department of Medicaid (ODM) updates
To stay up to date on ODM news, subscribe to the ODM Press.
ODM to roll out EVV claims processing changes in seven phases
The Ohio Department of Medicaid has begun the roll out of Electronic Visit Verification
(EVV) claims validation requirements for home health services that are billed to Ohio Medicaid to ensure claims requiring electronic visit verification have a matching EVV visit record upon submission. Claims that do not match will be denied.
A list of services and their execution dates, and a claims validation process flowchart can be found on ODM's website.
Tips for contacting the Ohio Medicaid Integrated Helpdesk
The Integrated Helpdesk (IHD) is a great resource to use when you run into an issue. It provides 24-hour, 7 days a week access to information regarding client eligibility, claim and payment status, and provider information. Read the useful tips here.
Important reminder: Update 1099 address information in the Provider Network Management module
It is important that providers update all 1099 address information in the Provider Network Management (PNM) module on a regular basis. Ensure all information is current, including extra address details like suite number, house/office number, etc. to reduce the chance of non-delivery by the postal service. Access the quick reference guides here.
New features implemented in the Ohio Medicaid Enterprise System
The New Features Implementation Overview outlines key changes for providers.
Medicaid agreement revalidations
To complete revalidation, visit PNM & Centralized Credentialing.
Ohio Department of Medicaid fraud warning
If your Medicaid patient is contacted for their personal information, advise them not to respond. Report it to the Ohio Attorney General at 1-800-282-0515 or via the online form.
Updated claim submission and adjudication FAQ
Claims and Prior Authorization Submission Frequently Asked Questions (FAQ)
|
|
|---|
|
Ohio Department of Medicaid email links
|
|
|---|
|
 Claims and billing Claims and billing |
|
|---|
|
New functionality - NaviNet® claims investigation attachments
AmeriHealth Caritas Ohio and NantHealth|NaviNet are excited to announce that we are bringing you a new feature: Claim Investigation Attachments. You can now upload supporting documents with your electronic claim investigation request within the NaviNet provider portal!
This enhancement is designed to streamline your workflow by eliminating the need to complete forms and fax/mail supporting documentation
Each supporting document will need to be 32 MB or smaller and in one of the following formats:
New to Claim Investigations in NaviNet?
Once logged into the portal, view the Claims investigation training video for a walk-through of the process.
New to NaviNet?
If you do not have access to the NaviNet provider portal, please visit: https://register.navinet.net/ to sign up.
If you have questions or need further assistance, contact the NaviNet Customer Support team at 1-888-482-8057, Monday through Friday, 8 a.m. to 11 p.m.
Sign up for multi-factor authentication by May 4
To increase protection of the provider network management system, the state has elected to require multi-factor authentication (MFA) when signing into the system. We encourage our providers to sign up for multi-factor authentication before the deadline of May 4 to prevent loss of access to the program.
The Ohio Department of Medicaid (ODM) and Sandata are preparing for the June 1 roll out of Electronic Visit Verification (EVV) claims validation requirements for Phase II and Phase III providers. Meeting these new claims validation obligations will ensure complete and accurate EVV data is matched to each claim submitted for reimbursement.
To help Phase II and III providers successfully comply, ODM has made a variety of resources available, including dedicated daily office hours, enhanced online user guides and EVV Claims Validation Process Flowchart.
Stay tuned to Ohio Medicaid’s Electronic Visit Verification webpage for more updates.
DentaQuest pre-payment review update
Effective March 1, the pre-payment review requirement was removed for procedure code D9230 (inhalation of nitrous oxide/analgesia, anxiolysis) for AmeriHealth Caritas Ohio Medicaid members ages 20 and under. Please be aware that this service is subject to medical necessity criteria and retrospective review. Although the narrative requirement has been removed, we strongly encourage providers to maintain documentation of medical necessity, which can be included in the claim submission.
If you have questions or need assistance, call the Ohio Provider Services line at 1-855-398-8411, reach out to your Provider Partner directly, or email the Provider Engagement team: OHProviderEngagement@DentaQuest.com.
Electronic data interchange
Providers with electronic data interchange (EDI) capabilities may submit claims, eligibility inquiries, claim status inquiries, and associated attachments by being a trading partner authorized by ODM or by contracting with an ODM-authorized trading partner. For more information, visit the ODM trading partners webpage or call the ODM IHD at 1-800-686-1516.
Direct Data Entry
For Direct Data Entry (DDE), providers should log in to Change Healthcare using the tool called ConnectCenter to improve claims management functionality. Providers who have a limited ability to submit claims through their hospital or project management system may now benefit from key features of the ConnectCenter tool. There is no cost to providers to use ConnectCenter. Learn more on our claims and billing webpage.
Connectivity restored with Optum/Change Healthcare
The restoration of connectivity with Optum/Change Healthcare gives our providers options for claims submissions. Click here to learn more about the electronic and manual/direct entry options.
Questions about reimbursement or payment policies?
Click the appropriate link below for detailed information.
No paper claims
The Next Generation of Ohio Medicaid program's guidelines require all claims to be submitted via the Electronic Data Exchange (EDI). Use AmeriHealth Caritas Ohio’s EDI Payer ID# 35374. You can get started on our website with claims how-tos, quick guides, links, and contact info.
Claims Payment Systemic Error report
The Claims Payment Systemic Errors (CPSE) report is updated and posted monthly on our website. AmeriHealth Caritas Ohio encourages you to review this log frequently and before contacting our Provider Services team. If you have additional questions, please reach out to Provider Services at 1-833-644-6001 and, as always, you can reach out to your local account executive.
Submitting claim disputes on NaviNet
If a provider disagrees with the outcome of a claim, the first step should always be to submit a claim dispute via fax or online. Below are the steps to submit a claim dispute on our NaviNet portal:
Although the dispute is being submitted online, all resulting correspondence will still be received via mail.
Providers can submit a dispute with attachments to AmeriHealth Caritas Ohio via NaviNet. Providers have the option to submit disputes through NaviNet, instead of faxing or mailing. We recommend providers use this option. Log into NaviNet, go to Forms & Dashboards, scroll down to Provider Disputes, then click on the Submit Provider Disputes link. Turnaround time is 15 days for disputes.
|
|
 Prior authorizations Prior authorizations |
|
|---|
|
Contact Utilization Management for a prior authorization prior to providing care to our members: 1-833-735-7700. Additionally, if interested in joining our network please reach out to our Contracting department via email at: providerrecruitmentoh@amerihealthcaritasoh.com. This email address can also be used by vision providers looking for in-network vendors who can provide eyeglass frames and lenses.
Submit prior authorization requests (PA) electronically through NaviNet
AmeriHealth Caritas Ohio offers our providers access to our Medical Authorizations portal for electronic authorization inquiries and submission. The portal is accessed through NaviNet and located on the Workflows menu.
In addition to submitting and inquiring on existing authorizations, you will also be able to:
- Verify if no authorization is required
- Receive auto approvals, in some circumstances
- Submit amended authorization
- Attach supplemental documentation
- Sign up for in-app status change notifications directly from the health plan
- Access a multi-payer authorization log
- Submit inpatient concurrent reviews online if you have health information exchange (HIE) capabilities (fax is no longer required)
- Review inpatient admission notifications and provide supporting clinical documentation
Submit all medical pharmacy prior authorizations (PA) to PerformRx
Prior authorization requests for prescriber administered medications should be submitted to PerformRx via fax. See our website for more information and the form.
|
|
 For behavioral health providers For behavioral health providers |
|
|---|
|
Questions regarding The American Society of Addiction Medicine Criteria Fourth Edition, Volume 1 – Adults
- Does ODM have a date in mind for adopting the Fourth Edition Criteria into Ohio Medicaid coverage and reimbursement policies? Given the extent of the changes included in the Fourth Edition, Volume 1 – Adults, the Department will not establish a timeline for implementation until it has completed the review and stakeholder engagement processes.
- What criteria will the managed care entities use when rendering a decision on a prior authorization request? Medicaid managed care entities will use the Third Edition Criteria when rendering a decision on a prior authorization request for SUD services until ODM formally adopts use of the Fourth Edition Criteria, Volume 1 – Adults. If a provider chooses to move towards the adoption of the Fourth Edition criteria prior to the State’s adoption, the provider must ensure that a request for PA meets the Third Edition criteria.
CEU opportunities
Sign up to receive email about AmeriHealth Caritas Ohio’s free Continuing Education Unit (CEU) opportunities.
Submitting prior authorization (PA) requests for behavioral health services
See the tip sheet for guidance on submitting PAs for behavioral health service requests.
|
|
Bright Start® maternity program
Bright Start helps our members stay healthy when they are pregnant and have a healthy baby. Members get access to our pregnancy care program to help schedule appointments and connect to community resources and additional programs. Visit the links below to learn more about this valuable program for your pregnant patients.
Care for pregnant members
Bright Start Welcome Booklet
Bright Start Beginnings Bundle
|
|
|---|
|
We are now covering doula services
AmeriHealth Caritas Ohio is dedicated to improving health outcomes for pregnant Medicaid members. Any pregnant or postpartum person with Medicaid coverage is eligible to receive doula services from a Board of Nursing-certified, Medicaid-enrolled doula. Doulas have been shown to improve birth outcomes, support birth equity, positively impact the social determinants of health, and reduce disparities in maternal and infant outcomes.
Click here to read the coverage overview, visit types, and find resources.
To read the Ohio Medicaid Managed Care Organizations Consolidated Doula Resource Guide click here.
The Ohio Board of Nursing has released a new State of Ohio Certified Doula FAQs document, providing key information on certification requirements, scope of practice and other essential details for doulas in Ohio.
|
|
|---|
|
 Resources and reminders Resources and reminders |
|
|---|
|
Sign up for this newsletter
Our monthly newsletter, Provider Partnerships, keeps you informed about plan news, updates, and resources. Click here to sign up.
Redeterminations
We understand that many members may be unaware that their redetermination period is approaching, and your engagement can play a crucial role in ensuring they take the necessary steps to avoid a lapse in coverage. We encourage our providers to remind their patients that they may need to complete the redetermination process to help ensure they can retain their Medicaid benefits. Please let us know how we can support you in sharing this important information. We appreciate your partnership and commitment to member health and continuity of care.
Provider resources
We highly recommend providers take a few minutes to familiarize themselves with the tools available on our website. Our user-friendly tools and resources are designed to support Ohio’s Medicaid providers and your staff in giving members excellent and efficient healthcare.
- prior authorization lookup tool
- video tutorials for claims submission
- step-by-step instructions for claims submission and our secure provider portal NaviNet
- Provider Manual
- Provider Claims and Billing Manual
- contact information for our call center and AmeriHealth Caritas Ohio provider services
- monthly CPSE reports and trending claims issue information
Updated HEDIS guidelines for the Care Gap Closure program
View the HEDIS 2024 Documentation and Coding Guidelines for care delivered in 2024.
Provider Network Management (PNM) portal
Until it is fully active, please continue to send roster updates to both PNM and the MCO’s. Behavioral Health providers ARE able to only update through the PNM portal without submitting rosters to the MCO’s.
Credentialing reminder
Providers no longer need to complete credentialing with each managed care organization. Credentialing is now completed through the state's PNM portal. More information can be found here.
|
|
 Training opportunities Training opportunities |
|
|---|
|
New provider orientation schedule
Join us for virtual New Provider Orientation sessions. They are an opportunity for us to introduce AmeriHealth Caritas Ohio, how we operate, what tools and opportunities we have available to our providers, and what sets us apart from the other managed care organizations in the state. You can schedule an individual orientation for yourself or your staff with your account executive or can attend one of the virtual group sessions.
Your personal AmeriHealth Caritas Ohio Account Executives look forward to meeting you! Click here to see the entire calendar and register.
|
|
|---|
|
Comprehensive Primary Care (CPC) quarterly webinar series
The 2025 CPC quarterly webinar series will focus on keeping practices informed about the latest CPC updates, learning opportunities, discussions and more. Topics will be sent out ahead of time. Click here to register.
These take place from 9:30 to 11 a.m. on the following dates:
- Tuesday, September 16
- Tuesday, November 18
|
|
|---|
|
2025 CPC summer learning session
Dates: July 15 and July 22
Time: 9:30 a.m. to 3:30 p.m.
Where: 4200 Surface Road, Columbus, OH 43228
Room: Willow/Walnut conference room
This session is taking place twice to maximize attendance; however, the same information is being shared at both. If you plan on attending, please only register for one of the two dates. More details will be sent via the CPC listserv.
|
|
|---|
|
Cultural competency training opportunities
AmeriHealth Caritas Ohio is committed to promoting education on and awareness of culturally and linguistically appropriate services (CLAS) and to combatting the effects of low health literacy on the health status of our members. |
|
|---|
|
Tell us a little bit about where you’re from and where you went to school.
I was born and raised in Dayton, Ohio. I went to Walter E. Stebbins High School and I attended Fortis College.
Everyone at AmeriHealth Caritas Ohio has a story about why they joined the team. What’s yours?
I heard great things about AmeriHealth Caritas. I have Medicaid
knowledge and an extensive medical background. I heard AmeriHealth Caritas Ohio was a growing company with great opportunities.
What drew you to this profession?
I found that I wanted to see healthcare from a different perspective and to feel like I was making a difference by helping people. I wanted to try something different. I have been working in healthcare since I was a senior in high school and worked as CMA for almost 11 years after that.
What do you like to do in your free time?
I love spending time with my 11-year-old son and doing things that interest him. I look for autistic-friendly events for him or family-friendly events that he and I can attend that will lead to resources and connections for us. When I have spare time, I model vintage clothing from the Silver Screen era and we spend time with my parents.

|
|
|
If you could have dinner with anyone in the world, dead or alive, who would it be? Why?
My parents, they are caring and knowledgeable, and the only support system my son and I have right now as we navigate through some of life’s obstacles.
What are 2 apps on your phone you CANNOT live without?
Facebook and
Instagram.
Any interesting facts about yourself that you’d like to share?
I collect vintage items - anything from clothing, shoes, accessories, to décor, etc.
|
|
|---|
|
April is Minority Health Month
Minority Health Month (MHM) was created by the Ohio Commission on Minority Health in April 1989 with the first celebration featuring community-initiated events. MHM was designed to be a 30-day inclusive, high-visibility, wellness campaign focusing on health promotion and disease prevention among minority populations. This year’s theme is Advancing Commitments to Eliminate Health Disparities.
The five goals of Minority Health Month are to:
|
|
|---|
|
- Provide crucial information to allow individuals to practice disease prevention
- Promote healthy lifestyles
- Showcase healthcare professionals and resources
- Highlight the unequal health of Ohio’s minorities compared to non-minorities
- Increase ongoing community support to improve minority health
|
|
|
|
|---|
|
AmeriHealth Caritas Ohio is committed to promoting education on and awareness of culturally and linguistically appropriate services (CLAS) and to combating the effects of low health literacy on the health status of our members. We have a collection of no-cost CME-accredited classes and resources that support continuing education in this area. |
|
|---|
|
Need help?
AmeriHealth Caritas Ohio Provider Services is ready to help.
|
|
|---|
|
|
|
|
|  |
|
|
|
|
