|
|
|
|
|
|
Provider Services 1-833-644-6001 |
|
|---|
|
|

Submit a 275 claims attachment transaction
AmeriHealth Caritas Ohio is accepting ANSI 5010 ASC X12 275 claim attachment transactions. The 275 attachments are accepted via Change Healthcare (Optum) and Availity. Please contact your Practice Management System Vendor or EDI clearinghouse to inform them that you wish to initiate electronic 275 claim attachment transaction submissions via 35374.
Availity
- There are two ways 275 claim attachments can be submitted:
After logging in, providers registered with Availity may access the Attachments - Training Demo for detailed instructions on the submission process via: Training Link apps.availity.com or refer to the Availity Claims Attachment Quick Reference guide located under Claims Resources at the bottom of this page.
Optum/Change Healthcare
- There are two ways 275 attachments can be submitted:
- Batch — You may either connect to Optum/Change Healthcare directly or submit via your EDI clearing house.
- API (via JSON) — You may submit an attachment for a single claim.
View the Change Healthcare 275 claims attachment transaction video for detailed instructions on this process.
General guidelines
- A maximum of 10 attachments are allowed per submission. Each attachment cannot exceed 10 megabytes (MB) and total file size cannot exceed 100MB.
- The acceptable supported formats are pdf, tif, tiff, jpeg, jpg, png, docx, rtf, doc, and txt.
- The 275 attachments must be submitted prior to the 837. After successfully submitting a 275 attachment, an Attachment Control Number will generate. The Attachment Control Number must be submitted in the 837 transactions as followed:
- CMS 1500
- Field Number 19
- Loop 2300
- PWK segment
-
- UB-04
- Field Number 80
- Loop 2300
- PWK01 segment
- In addition to the Attachment Control Number, the following 275 attachment report codes must be reported in field 19 of the CMS 1500 or field number 80 of the UB-04 (see grid below).
|
Attachment Type
|
Claim assignment attachment report code
|
|
Itemized Bill
|
03
|
|
Medical Records for HAC review
|
M1
|
|
Single Case Agreement (SCA)/LOA
|
04
|
|
Advanced Beneficiary Notice (ABN)
|
05
|
|
Consent Form
|
CK
|
|
Manufacturer Suggested Retail Price/Invoice
|
06
|
|
Electric Breast Pump Request Form
|
07
|
|
CME Checklist consent forms (Child Medical Eval)
|
08
|
|
EOBs — for 275 attachments should only be used for non-covered or exhausted benefit letter
|
EB
|
|
Certification of the Decision to Terminate Pregnancy
|
CT
|
|
Ambulance Trip Notes/Run Sheet
|
AM
|
Questions
If you have questions about this communication, please contact your Provider Account Executive or the Provider Services Department at 1-833-644-6001.
|
|
|---|
|
Ohio Department of Medicaid (ODM) updates
To stay up to date on ODM news, subscribe to the ODM Press.
Extended: timely filing notice
Following an analysis of claims data ODM has determined it necessary to extend the timely filing deadline to March 1, 2025. To ensure a consistent experience for providers of Medicaid services, AmeriHealth Caritas Ohio will follow this guidance and extend the deadline.
New features implemented in the Ohio Medicaid Enterprise System
The New Features Implementation Overview outlines key changes for providers.
Medicaid agreement revalidations
To complete revalidation, visit PNM & Centralized Credentialing.
Ohio Department of Medicaid fraud warning
If your Medicaid patient is contacted for their personal information, advise them not to respond. Report it to the Ohio Attorney General at 1-800-282-0515 or via the online form.
Updated claim submission and adjudication FAQ
Claims and Prior Authorization Submission Frequently Asked Questions (FAQ)
|
|
|---|
|
Ohio Department of Medicaid email links
|
|
|---|
|
 Claims and billing Claims and billing |
|
|---|
|
Connectivity restored with Optum/Change Healthcare
The restoration of connectivity with Optum/Change Healthcare gives our providers options for claims submissions. Click here to learn more about the electronic and manual/direct entry options.
Questions about reimbursement or payment policies?
Click the appropriate link below for detailed information.
NaviNet - submitting disputes with attachments
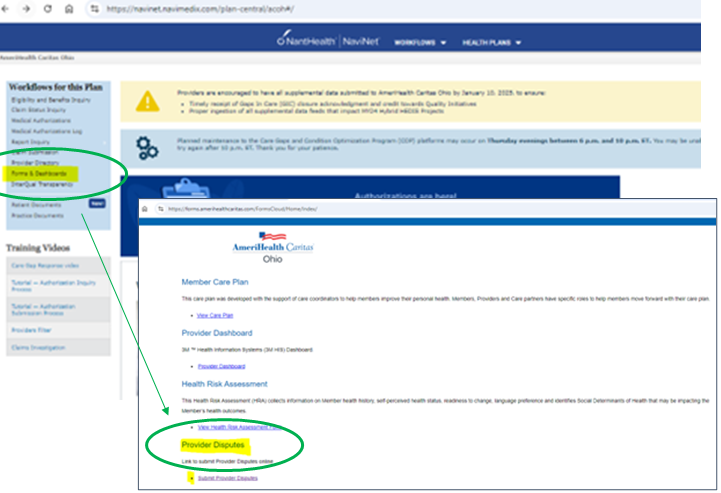
Providers can submit a dispute with attachments to AmeriHealth Caritas Ohio via NaviNet, instead of faxing or mailing. WE RECOMMEND PROVIDERS USE THIS OPTION. Log into NaviNet, go to Forms & Dashboards, scroll down to Provider Disputes, then click on the Submit Provider Disputes link. Turnaround time is 15 days for disputes.
How to investigate a claim
- Log into NaviNet.
- On the Health Plans menu, under My Plans, click AmeriHealth Caritas Ohio.
- Under Workflows for This Plan, click Claim Status Inquiry, and then find your claim.
- On the Claim Details screen, above the status bar, click Claim Investigation. The Investigation Claim # pop-up window appears.
- Choose an investigation type, and then type your comments for the investigation reviewers. Claim investigations are per claim, not per line item. To reference a specific claim line, provide the line number in the Comments box.
- In the remaining boxes, type your contact information for this investigation so that customer service can contact you, if necessary.
- Click Submit.
A confirmation message appears. For example:
Your Investigation Request for Claim # 118833994 has been submitted to the plan.
Our goal is to respond to your inquiry within 15 days, however, at times due to the complexity of your issue our response may take more time. If your inquiry takes more than 15 days to resolve, AmeriHealth Caritas Ohio will provide an update every five days until your issue is resolved.
To check the status of your investigation after you submit it, click Claim Investigation Inquiry under Workflows for This Plan.
If you submit an investigation without required information, AmeriHealth Caritas Ohio cannot complete it. AmeriHealth Caritas Ohio responds to the investigation and notes any missing information. Click here for the NantHealth Help Center.
No paper claims
The Next Generation of Ohio Medicaid program's guidelines require all claims to be submitted via the Electronic Data Exchange (EDI). Use AmeriHealth Caritas Ohio’s EDI Payer ID# 35374. You can get started on our website with claims how-tos, quick guides, links, and contact info.
Correcting claims
What if I submitted claims with the wrong rate or CPT code? Please refer to our Provider Claims and Billing Manual on how to submit corrected claims on page 52.
Claims Payment Systemic Error (CPSE) report
The Claims Payment Systemic Errors (CPSE) report is updated and posted monthly on our website. AmeriHealth Caritas Ohio encourages you to review this log frequently and before contacting our Provider Services team. If you have additional questions, please reach out to Provider Services at 1-833-644-6001 and, as always, you can reach out to your local account executive.
Diabetes self-management education enhanced reimbursement rates
AmeriHealth Caritas Ohio and the Ohio Managed Care Organizations (MCOs) are working collaboratively to make diabetes management easier for providers and their patients. Diabetes education and support for the use of continuous glucose monitors (CGMs) have proven to be effective in diabetes care management.
To facilitate increased utilization of these enhanced tools, AmeriHealth Caritas Ohio and the other MCOs will pay an enhanced rate to providers rendering Diabetes Self-Management Education (DSME) and billing the appropriate codes: G0108 and G0109. In addition, PA is not required for members who receive a covered CGM device through durable medical equipment (DME) providers or through their pharmacy. Providers must use HCPCS codes A4239 and E2103 for CGMs provided through DME.
For additional information regarding these updates, including who to contact at each MCO for questions, see the quick reference guide on our provider website.
|
|
 Prior authorizations Prior authorizations |
|
|---|
|
Contact Utilization Management for a prior authorization prior to providing care to our members: 1-833-735-7700. Additionally, if interested in joining our network please reach out to our Contracting department via email at: providerrecruitmentoh@amerihealthcaritasoh.com. This email address can also be used by vision providers looking for in-network vendors who can provide for eye glass frames and lenses.
Submit prior authorization requests (PA) electronically through NaviNet
AmeriHealth Caritas Ohio offers our providers access to our Medical Authorizations portal for electronic authorization inquiries and submission. The portal is accessed through NaviNet and located on the Workflows menu.
In addition to submitting and inquiring on existing authorizations, you will also be able to:
- Verify if No Authorization is Required
- Receive Auto Approvals, in some circumstances
- Submit Amended Authorization
- Attach supplemental documentation
- Sign up for in-app status change notifications directly from the health plan
- Access a multi-payer Authorization log
- Submit inpatient concurrent reviews online if you have Health Information
- Exchange Health Information Exchange (HIE) capabilities (fax is no longer required)
- Review inpatient admission notifications and provide supporting clinical documentation
Submit all medical pharmacy prior authorizations (PA) to PerformRx
Prior authorization requests for prescriber administered medications should be submitted to PerformRx via fax. See our website for more information and the form.
|
|
For Behavioral Health Providers
CEU opportunities
Sign up to receive email about AmeriHealth Caritas Ohio’s free continuing education unit (CEU) opportunities.
Ohio Department of Medicaid Introduces Mental Health Peer Support Services
New service added to the growing list of behavioral health resources available to Ohioans.
Submitting prior authorization (PA) requests for behavioral health services
See the new tip sheet for guidance on submitting PAs for behavioral health service requests.
Statewide registry of recovery housing residences
The Ohio Department of Mental Health and Addiction Services released a public-facing registry of recovery homes in early November. Starting January 1, 2025, only homes on this registry may receive referrals from mental health and addiction services providers. Providers should check this registry and ensure that any homes that they regularly refer individuals to are listed on the registry. If they are not, those individuals need to take the needed steps to ensure that they are on the registry by January 1, 2025. Only homes that are appropriately accredited may be on the registry. The two entities that are providing the accreditation are Ohio Recovery Housing, which offers a certification, and Oxford House, which charters recovery homes. For more information contact Ohio Recovery Housing at 1-614-453-5133 or visit info@ohiorecoveryhousing.org.
|
|
|---|
|
 Resources and reminders Resources and reminders |
|
|---|
|
Updated HEDIS guidelines for the Care Gap Closure program
View the HEDIS 2023 Documentation and Coding Guidelines for care delivered in 2024.
PNM portal
Until it is fully active, please continue to send roster updates to both PNM and the MCO’s. Behavioral Health providers ARE able to only update through the PNM portal without submitting rosters to the MCO’s.
Credentialing reminder
Providers no longer need to complete credentialing with each managed care organization. Credentialing is now completed through the state's PNM portal. More information can be found here.
|
|
 Training opportunities Training opportunities |
|
|---|
|
New Provider Orientation Schedule
You and your office staff are invited to join us for a virtual New Provider Orientation session. These orientations are designed not only to familiarize you with the vast resources available to you through our website, but also to identify areas of importance to help you work with us to best serve our members — your patients.
Your personal AmeriHealth Caritas Ohio Account Executives look forward to meeting you! Click here to see the entire calendar and register.
Don't forget to complete the attestation once you attend a session. The Ohio Department of Medicaid requires us to maintain a registry for the New Provider Orientation attendance.
|
|
|---|
|
Cultural competency training
AmeriHealth Caritas Ohio is committed to promoting education on and awareness of culturally and linguistically appropriate services (CLAS) and to combatting the effects of low health literacy on the health status of our members. There are several training opportunities on our website. |
|
|---|
|
December is National Influenza Awareness Month
December is a time dedicated to reminding people that getting an influenza (flu) vaccine will help fight the flu. It is a call to all Americans six months and older to get their annual flu vaccine if they have not already.
The U.S. Centers for Disease Control and Prevention (CDC) advises as a healthcare professional, your strong recommendation is a critical factor in whether your patients get an influenza vaccine. Most adults believe vaccines are important, but they need a reminder from you to get vaccinated. After making your recommendation, follow up with each patient during subsequent appointments to ensure they received an influenza vaccine. If a patient still is unvaccinated, repeat the recommendation and try to identify and address any questions or concerns.
The CDC has guidance for healthcare providers for the prevention, diagnosis, and treatment of influenza. Click here to learn more.
|
|
|---|
|
Need help?
AmeriHealth Caritas Ohio Provider Services is ready to help.
|
|
|---|
|
|
|
|
|  |
|
|
|
|
