|
|
|
|
|
|
Provider Services 1-833-644-6001 |
|
|---|
|
|
AmeriHealth Caritas Ohio Earns NCQA Health Plan Accreditation
Demonstrating its commitment to improving the health of Ohioans most in need, AmeriHealth Caritas Ohio has earned health plan accreditation from the National Committee for Quality Assurance (NCQA).
“We embrace Ohio Department of Medicaid’s goals for its Next Generation of Medicaid Managed Care: improving wellness and health outcomes, emphasizing a personalized care experience, supporting providers in better patient care, improving care for those with complex needs, and increasing transparency and accountability. Meeting NCQA’s high accreditation standards shows that we share the department’s desire to build a Medicaid program that better serves the Ohioans who need it,” said AmeriHealth Caritas Ohio Market President and CEO Mark Grippi.
|
|
AmeriHealth Caritas Ohio and Zest Pediatric Network honored
AmeriHealth Caritas Ohio is honored to accept the Pinnacle Award from the Ohio Association of Health Plans (OAHP). OAHP recognized us for the Zest Pediatric Network program- bringing concierge care to our youngest Medicaid members in northeast Ohio. Concierge care means Zest pediatricians are available 24/7, offering select in-home visits, direct access to doctors, no-rush, and convenient appointment times. "This program is special because we are taking the concept of concierge care - that often comes with a significant cost to patients - and making it available to Ohioans who need it most," said Mark Grippi, AmeriHealth Caritas Ohio CEO, and market president.

Pictured L-R: Greg LaManna (CEO, Anthem Blue Cross & Blue Shield Medicaid Health Plan Ohio), Mark Grippi (AmeriHealth Caritas Ohio, Market President/CEO), Suzette Heitkamp (AmeriHealth Caritas Ohio, Market CFO), Dr. Andrew Hertz (President, Zest Pediatric Network). Not pictured: Robert Metzler (AmeriHealth Caritas Ohio, Manager Provider Network Management) |
|
|---|
|
275 claim attachment transaction is now available via Availity
AmeriHealth Caritas Ohio is accepting ANSI 5010 ASC X12 275 claim attachment transactions (unsolicited) via Availity.
Please contact your Practice Management System Vendor or EDI clearinghouse to inform them that you wish to initiate electronic 275 claim attachment transaction submissions for payer ID: 84243.
A maximum of ten attachments are allowed per submission. Each attachment cannot exceed 10 megabytes (MB) and total file size cannot exceed 100MB. The acceptable supported formats are pdf, tif, tiff, jpeg, jpg, png, docx, rtf, doc, and txt.
There are two ways 275 claim attachment transactions can be submitted:
For instructions accessing the Attachments Training Demo, visit https://www.amerihealthcaritasoh.com/provider/newsletters-and-updates/index.aspx.
If you have questions, please contact Availity Client Services at 1-800-AVAILITY (282-4548). Assistance is available Monday through Friday from 8 a.m. to 8 p.m.
|
|
|---|
|
Submitting disputes with attachments via NaviNet
As of 8/29/24 providers can now submit a dispute with attachments to AmeriHealth Caritas Ohio via NaviNet. To access, go to the Plan Central Home page, Forms and Dashboards and select Provider Disputes.
|
|
|---|
|
Ohio Department of Medicaid updates
To stay update to date on ODM news, subscribe to the ODM Press.
Check out the updated MyCare Ohio Webpage on Medicaid.ohio.gov!
MyCare Ohio is the managed care program designed for Ohioans who receive both Medicaid and Medicare benefits. The MyCare Ohio program integrates Medicaid and Medicare benefits into one program, coordinated by a managed care plan.
To make it easier for you to find the information you need, visit the updated MyCare Ohio webpage.
The Ohio Department of Medicaid is conducting a series of MyCare Ohio program community input sessions to hear about your experiences navigating the current MyCare Ohio program. To learn more about the MyCare Ohio program and community input sessions and view the schedule, please visit the MyCare Ohio program webpage.
Doula trainings
The Ohio Department of Medicaid, the Ohio Board of Nursing, and Medicaid Managed Care Organizations (MCO), will be hosting a training series for doulas. Those interested in providing certified doula services within the State of Ohio, with the intent to serve Ohio Medicaid members, are encouraged to attend. Registration for the training series can be found on the ODM doula webpage.
- Training session 2: Thursday, September 26 from 10 a.m.-12 p.m.
- MCO 101 and contracting process
- Training session 3: Tuesday, October 29 from 1:30 p.m.-3:30 p.m.
- MCO claims billing and prior authorization process
- Training session 4: Thursday, November 7 from 10 a.m.-12 p.m.
- Fee-for-service billing and prior authorization process
- Training session 5: Thursday, November 21 from 12:30 p.m.-2 p.m.
- Related maternal health topics overview
2024 Comprehensive Primary Care (CPC) Webinar Series with ODM
ODM will virtually share program updates, resources, best practices, and more on 11/14. Click here to register.
Free CPTII Coding Training
As part of the all-MCO CPT II Workgroup initiative, we would like to announce an upcoming virtual training presented by ArchProCoding. This is an EMR agnostic beginning-level training, meant to identify best practices related to how clinical providers accurately document their care and diagnoses. We are also excited to announce that there will be an opportunity for CEUs provided with this training.
This 90-minute training will be offered on 9/25 at 2 p.m.
If you have questions or would like to be added to the communication list for this training, please email MHOVBR@molinahealthcare.com. We hope to see you there!
|
|
|---|
|
Ohio Department of Medicaid Resources
New features implemented in the Ohio Medicaid Enterprise System
The New Features Implementation Overview outlines key changes for providers.
Medicaid’s Office of Behavioral Health Policy 2024 rate increases
Medicaid agreement revalidations
To complete revalidation, visit PNM & Centralized Credentialing.
SL modifier not required for Vaccines for Children (VFC) Program
As of April 30, the VFC program no longer requires the use of the SL modifier for claims reimbursement.
Ohio Department of Medicaid fraud warning
If your Medicaid patient is contacted for their personal information, advise them not to respond. Report it to the Ohio Attorney General at 1-800-282-0515 or via the online form.
Updated claim submission and adjudication FAQ
Claims and Prior Authorization Submission Frequently Asked Questions (FAQ)
|
|
|---|
|
Ohio Department of Medicaid email links
|
|
|---|
|
 Resources and reminders Resources and reminders |
|
|---|
|
Need help?
Access and availability standards
As part of ongoing network management, periodic outreach to confirm maintenance of access and availability standards does occur. The specific access time frames are determined by the provider type of the service and is outlined starting on page 33 of the AmeriHealth Caritas Ohio Provider Manual.
Updated HEDIS guidelines for the Care Gap Closure program
View the HEDIS 2023 Documentation and Coding Guidelines for care delivered in 2024.
PNM portal
Until it is fully active, please continue to send roster updates to both PNM and the MCO’s. Behavioral Health providers ARE able to only update through the PNM portal without submitting rosters to the MCO’s.
Credentialing reminder
As of the launch of the next gen of Medicaid on 2/1/2023 providers no longer need to complete credentialing with each managed care organization. Credentialing is now completed through the state's PNM portal. More information can be found here.
|
|
 Prior authorizations Prior authorizations |
|
|---|
|
Procedure code authorization Q3
To enhance the provider experience by making it easier for providers to navigate the prior authorization process, AmeriHealth Caritas Ohio has made changes to Prior Authorization requirements. Please click here to see the updates.
Note: prior authorization requests for prescriber administered medications should be submitted to PerformRx via fax. See our website for more information and the form.
Out of network providers
Contact Utilization Management for a prior authorization prior to providing care to our members: 1-833-735-7700. Additionally, if interested in joining our network please reach out to our Contracting department via email at: providerrecruitmentoh@amerihealthcaritasoh.com. This email address can also be used by vision providers looking for in-network vendors who can provide for eye glass frames and lenses.
Submitting prior authorization (PA) requests for behavioral health services
See the new tip sheet for guidance on submitting PAs for behavioral health service requests.
Submit prior authorization requests (PA) electronically through NaviNet
AmeriHealth Caritas Ohio offers our providers access to our Medical Authorizations portal for electronic authorization inquiries and submission. The portal is accessed through NaviNet and located on the Workflows menu.
In addition to submitting and inquiring on existing authorizations, you will also be able to:
- Verify if No Authorization is Required
- Receive Auto Approvals, in some circumstances
- Submit Amended Authorization
- Attach supplemental documentation
- Sign up for in-app status change notifications directly from the health plan
- Access a multi-payer Authorization log
- Submit inpatient concurrent reviews online if you have Health Information
- Exchange (HIE) capabilities (fax is no longer required)
- Review inpatient admission notifications and provide supporting clinical documentation
Submit all medical pharmacy prior authorizations (PA) online
Prior authorization requests for prescriber administered medications should be submitted to PerformRx via fax. See our website for more information and the form.
Prior authorization lookup tool
As a reminder, to verify whether a service requires prior authorization, use the Prior Authorization Lookup Tool on the provider website.
NOTE: Prescriber-administered medications that are billed via the medical benefit (CMS 1500 or UB-04) are reviewed by our PBM, PerformRx. Prior authorization request for prescriber administered medications should be submitted to PerformRX via fax. You can download a form here to submit via fax.
Questions? Contact your Provider Network Management Account Executive or Provider Services at 1-833-644-6001.
|
|
 Claims and billing Claims and billing |
|
|---|
|
Help with claim disputes that are UPHELD
When a provider files a claim dispute and receives an Upheld Letter there is a Service FORM number – on this document. Please provide this to your account executive when reaching out to the Provider Services Call Center to research your issue.
Helpful hint: reference numbers for provider requests
There may be instances, when a Provider disagrees with the outcome of a dispute/appeal. In order to exhaust all options, the Provider can request that their assigned Account Executive further research the issue. Please be aware that your Account Executive will need a reference number (referred to as an SF ID#) to have the issue reviewed. The SF ID# can be located on the decision resolution notice sent by AmeriHealth Caritas Ohio. See example below.
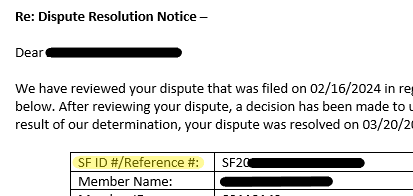
Please document this reference number when received, as it is the best way to locate previously submitted issues. These reference numbers are also created for roster changes, among other types of Provider requests, and will always be helpful in locating status updates or requesting further research.
How to investigate a claim
- Log into NaviNet.
- On the Health Plans menu, under My Plans, click AmeriHealth Caritas Ohio.
- Under Workflows for This Plan, click Claim Status Inquiry, and then find your claim.
- On the Claim Details screen, above the status bar, click Claim Investigation. The Investigation Claim # pop-up window appears.
- Choose an investigation type, and then type your comments for the investigation reviewers. Claim investigations are per claim, not per line item. To reference a specific claim line, provide the line number in the Comments box.
- In the remaining boxes, type your contact information for this investigation so that customer service can contact you, if necessary.
- Click Submit.
A confirmation message appears. For example:
Your Investigation Request for Claim # 118833994 has been submitted to the plan.
Our goal is to respond to your inquiry within 7 days, however, at times due to the volume of complexity our response may take up to 30 days.
To check the status of your investigation after you submit it, click Claim Investigation Inquiry under Workflows for This Plan.
If you submit an investigation without required information, AmeriHealth Caritas Ohio cannot complete it. AmeriHealth Caritas Ohio responds to the investigation and notes the missing information. Click here for the NantHealth Help Center.
No paper claims
The Next Generation of Ohio Medicaid program's guidelines require all claims to be submitted via the Electronic Data Exchange (EDI). Use AmeriHealth Caritas Ohio’s EDI Payer ID# 35374. You can get started on our website with claims how-tos, quick guides, links and contact info.
Correcting claims
Oops! What if I submitted claims with the wrong rate or CPT code? Please refer to our Provider Claims and Billing Manual on how to submit corrected claims on page 52.
Provider Claims and Billing Manual - Box 33, no PO Box allowed
Field: 33
Field description: Billing provider Info and phone number
Required - identifies the provider that is requesting to be paid for the services rendered and should always be completed. Enter the physical location; PO Boxes are not acceptable.
- Required fields must be completed on all claim
- Loop ID: 2010AA
- Segment: NM103, NM104, NM105, NM107, N301, N401, N402, N403, PER04.
See page 17 of the Provider Claims and Billing Manual.
Claims Payment Systemic Error (CPSE) report
The Claims Payment Systemic Errors (CPSE) report is updated and posted on the Alerts and Newsletter page monthly. AmeriHealth Caritas Ohio encourages you to review this log frequently and before contacting our Provider Services team. If you have additional questions, please feel free to reach out to Provider Services at 1-833-644-6001 and, as always, you can reach out to your local account executive.
Diabetes self-management education enhanced reimbursement rates
AmeriHealth Caritas Ohio and the Ohio Managed Care Organizations (MCOs) are working collaboratively to make diabetes management easier for providers and their patients. Diabetes education and support for the use of continuous glucose monitors (CGMs) have proven to be effective in diabetes care management.
To facilitate increased utilization of these enhanced tools, AmeriHealth Caritas Ohio and the other MCOs will pay an enhanced rate to providers rendering Diabetes Self-Management Education (DSME) and billing the appropriate codes: G0108 and G0109. In addition, PA is not required for members who receive a covered CGM device through durable medical equipment (DME) providers or through their pharmacy. Providers must use HCPCS codes A4239 and E2103 for CGMs provided through DME.
For additional information regarding these updates, including who to contact at each MCO for questions, see the quick reference guide on our provider website.
|
|
Appeal/Dispute Reference Guide - Ohio Definitions
|
|
|---|
|
When should the provider submit an Appeal vs. Dispute? |
|
|---|
|
|
Item and Definitions
|
Timeframe
|
Contact Information
|
|
Appeal
Filed by the member or provider on behalf of the member (with a waiver), related to a denied Service/IP service (Prior Auth denials, Limit to service/Auth) when there is no claim on file.
|
60 days from the date of denial letter sent by UM.
|
Medical appeals may be submitted via:
Mail: AmeriHealth Caritas Ohio
Attn: Member Appeals Coordinator
PO Box 7346
London, KY 40742
Phone: AmeriHealth Caritas Ohio Member Services
1-833-764-7700
(TTY: 1-833-889-6446)
Secure contact form: https://apps.amerihealthcaritasoh.com/securecontact/index.aspx
|
|
Inquiry
Provider asking for more information on a claim and how it was processed.
|
None
If determined the claim can be adjusted, then the inquiry is a dispute and should follow that timeframe.
|
NaviNet portal (www.navinet.net)
|
|
Dispute (or Provider Claim Appeal)
Provider disagreeing with the way a claim was processed, paid, or denied.
ODM outlines the following categories of items that are considered a dispute:
- Claim Status
- Eligibility
- Other insurance
- Improper claim submission
- Overpaid/underpaid
- Provider not eligible to provide service
- Payment amount clarification
- Provider not credentialed
- Duplicate claim
- Timely filing
- Documentation issues
- Recoupments
- Prior Authorization
- Medical Necessity
- Level of Care (LOC)
- Non-covered services
- Provider affiliation
- Payment not received
- Patient Liability
- Sterilization/Hysterectomy consent form
- Past Dispute Timeframe
|
12 months from the DOS or 60 days from the EOB date.
|
Disputes may be submitted via:
Phone: 1-833-644-6001 (Select the prompts for the correct department and then select the prompt for claim issues).
NaviNet portal: https://navinet.secure.force.com/ with the claims adjustment inquiry function.
Mail: The request must include a copy of the dispute resolution letter.
AmeriHealth Caritas Ohio
Attn: Provider Claim Inquiry Team
PO Box 7126
London, KY 40742
Fax: 1-833-216-2272
|
|
|
|---|
|
Access the Provider Dispute Submission Form (PDF) |
|
|---|
|
AmeriHealth Caritas Ohio offers a novel approach to reach communities we serve
Our Mobile Wellness and Opportunity Center can come to your community! Depending on availability and established criteria, you can work with AmeriHealth Caritas Ohio to
conduct classes, wellness events, or health education within and around the bus.
The mobile unit is equipped with kiosks where attendees can access computers and a private location where providers can perform health screenings and engage personally with members.
We are pleased to offer this convenience at no cost to you and your community. We welcome the chance to collaborate with you to help people get care, stay well, and build healthy communities.
For more information or to reserve time with the Mobile Wellness and Opportunity Center, click to complete the request form or email us at Comms@AmeriHealthCaritasOH.com.
|
|
|---|
|
 Training opportunities Training opportunities |
|
|---|
|
Provider orientation
We encourage our new providers to attend one of our virtual orientation sessions. These offer us the opportunity to welcome you, introduce ourselves, and share our unique member benefits, value-based care program, claims and billing information and our provider portal, NaviNet. Join your personal account executives online or contact your local Account Executive to schedule an individual orientation. Click here to see the entire calendar and register.
Don't forget to complete the attestation once you attend a session. The Ohio Department of Medicaid requires us to maintain a registry for the New Provider Orientation attendance.
|
|
|---|
|
Cultural competency training
AmeriHealth Caritas Ohio is committed to promoting education on and awareness of culturally and linguistically appropriate services (CLAS) and to combatting the effects of low health literacy on the health status of our members. There are several training opportunities on our website. |
|
|---|
|
Pain Self-Management Education (PSME) is in full swing!
PSME is a four-session educational program for adults living with chronic non-cancer pain. PSME teaches pain self-management, healthy lifestyle, mindfulness, and healthy coping skills, with the goal of empowering people to live full and productive lives with pain.
This program is offered in collaboration with Meridian HealthCare at no cost to adults 18+ living with chronic pain and insured by ANY Ohio Medicaid plan.
To refer to this program, please direct patients to contact Meridian HealthCare directly at 1-330-797-0070 or email chronicpain@meridianhealthcare.net. Additional program information and referral flyers can be obtained by contacting Jhilleary@AmeriHealthCaritasOH.com.
|
|
|---|
|
Ask a Sandata trainer
Do you have questions about Electronic Visit Verifications (EVV)? You can schedule a private Zoom session with a Sandata trainer to discuss your EVV questions. The sessions cover: improving claims matching, solving reoccurring exceptions, and getting started with EVV.
|
|
|---|
|
Tell us a little bit about where you’re from and where you went to school.
I grew up in the SW suburbs of Cleveland in a small town called Berea. It is home of the legendary Cleveland Browns training facility. I graduated with
a bachelor's degree in Business Management from Malone University in Canton, also home of the Pro Football Hall of Fame.
Everyone at AmeriHealth Caritas Ohio has a story about why they joined the team. What’s yours?
I have
served in multiple roles in the healthcare industry, from working in the emergency room, IT and healthcare insurance sales, Director of Business Development predominantly in hospital systems to the healthcare insurance industry. Joining AmeriHealth Caritas Ohio in my current role allowed me to continue and serve those in communities less fortunate than most.
What drew you to this profession?
I started my career in professional sales within the technology field but wanted to make a difference in the quality of life for others to improve their healthcare and well-being.
What do you like to do in your free time?
Exercise, travel, automobile enthusiast, attend plays, concerts, and dabble in photography.
If you could have dinner with anyone in the world, dead or alive, who would it
be? Why?
Abe Lincoln because he abolished slavery.
|
|
|
What are 2 apps on your phone you CANNOT live without?
A weather app and Shazam.
Any interesting facts about yourself that you’d like to share?
I ran to Canada and back and have owned well over one hundred cars.


Ray DeAngelis
Provider Network Account Executive II
rdeangelis@amerihealthcaritasoh.com
Mobile: 1-440-829-9533 |
|
|---|
|
September is National Suicide Prevention Month
This month is a time to remember the lives lost to suicide, acknowledge the millions more who have experienced suicidal thoughts, and the many individuals, families and communities that have been impacted by suicide. It’s also a time to raise awareness about suicide prevention and share messages of hope.
During September, and throughout the year, we can care about suicide prevention; connect to community, culture, data, and research; and collaborate with others to address this public health problem that has impacted millions of Americans.
How You Can Help
Educate yourself and others about suicide prevention: Learn the warning signs and risk factors for suicide, how to support someone considering suicide, and familiarize yourself with the 988 Suicide & Crisis Lifeline.
|
|
Need help?
AmeriHealth Caritas Ohio Provider Services
|
|
|---|
|
|
|
|
|  |
|
|
|
|
